Category: Sensors
-
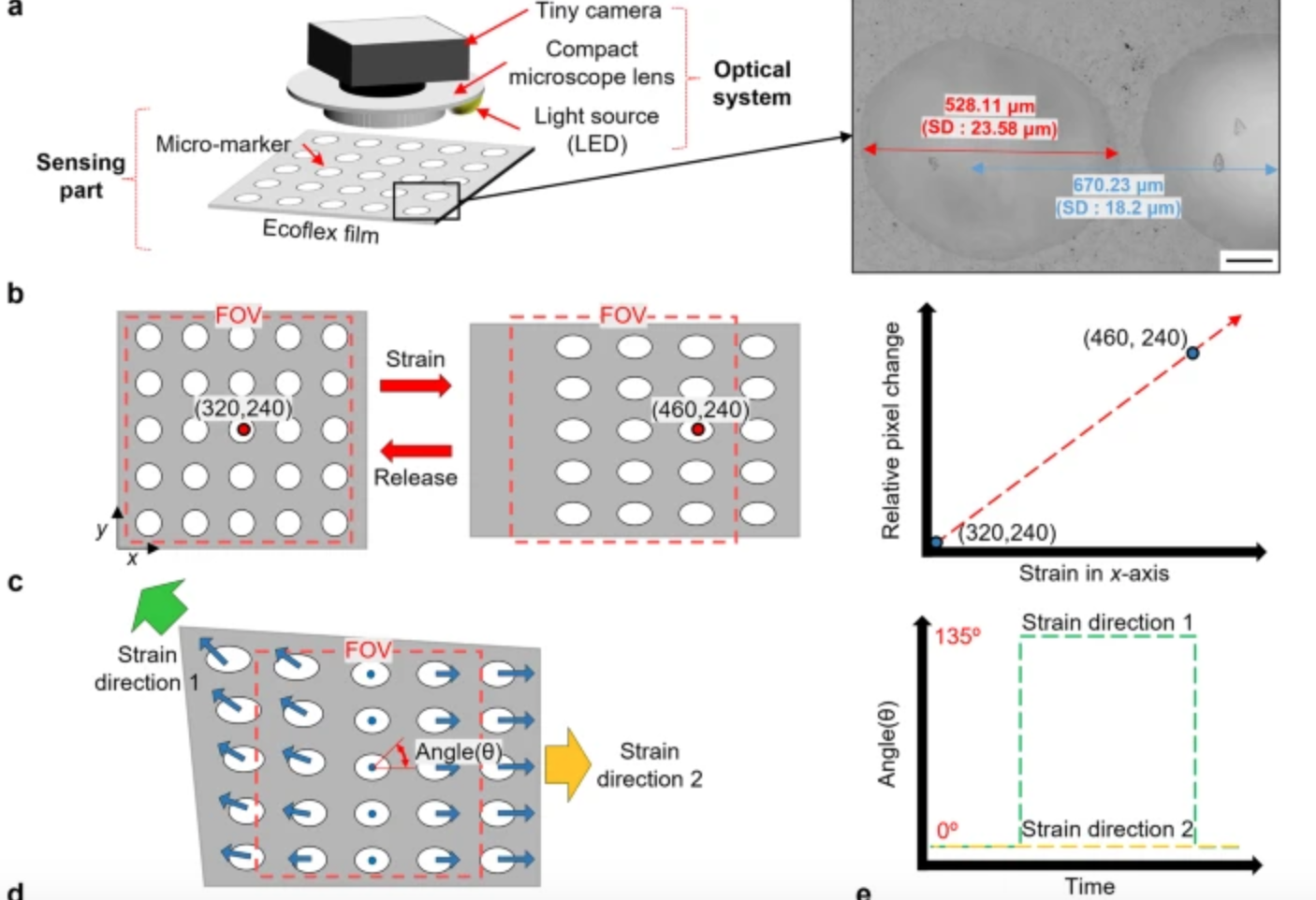
Computer vision enhanced sensors improve rehabilitation
POSTECH professor Sung-Min Park and researcher Sunguk Hong have developed optical sensor technology, integrated with computer vision, to track muscle movements in rehab patients with limited mobility. The sensors are flexible, lightweight, and able to gauge subtle body changes, while overcoming the conventional challenges of soft strain sensors – inadequate durability due to temperature and…
-
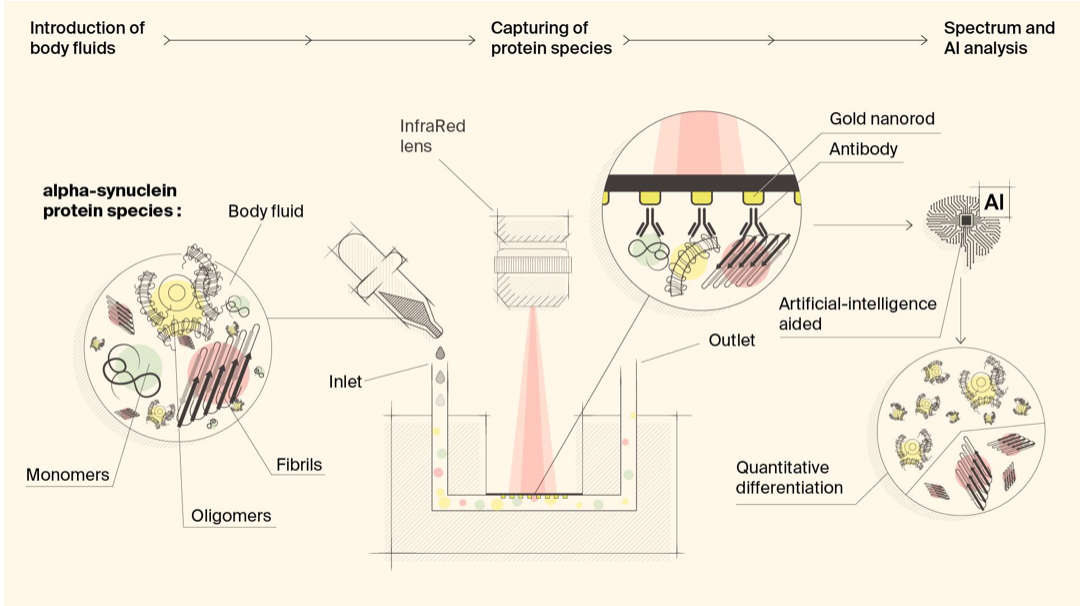
Biosensor detects misfiled proteins in Parkinson’s and Alzheimer’s disease
Hatice Altug, Hilal Lashue, and EPFL colleagues have developed ImmunoSEIRA, an AI-enhanced, biosensing tool for the detection of misfolded proteins linked to Parkinson’s and Alzheimer’s disease. The researchers also claim that neural networks can quantify disease stage and progression. The technology holds promise for early detection, monitoring, and assessing treatment options. Protein misfolding has been…
-
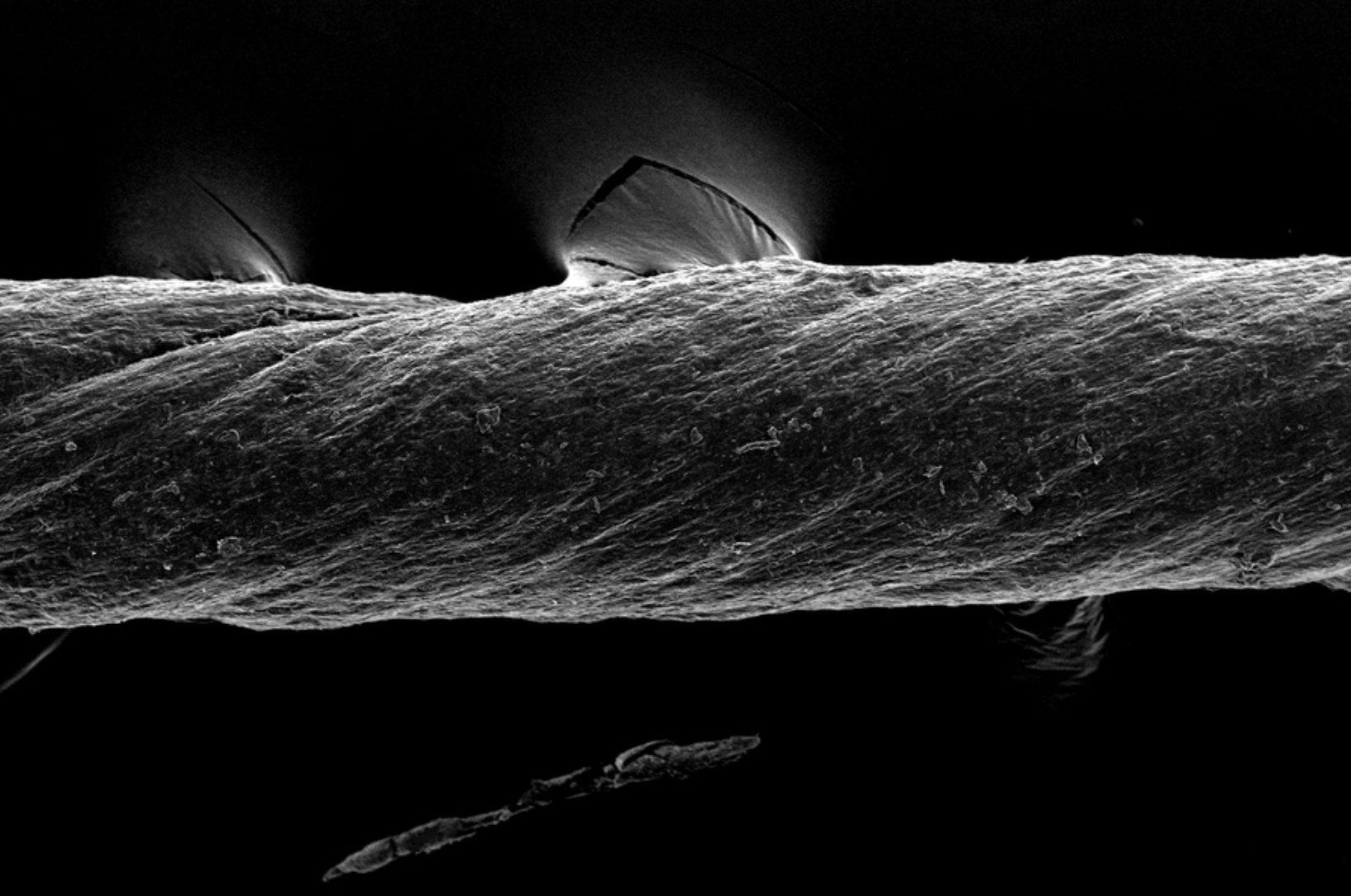
Hydrogel-coated sutures sense inflammation, can deliver drugs and stem cells
Giovanni Traverso has designed tough, absorbable, hydrogel-coated sutures, which in addition to holding post-surgery or wound-affected tissue in place, can sense inflammation and deliver drugs, including monoclonal antibodies. They could also be used to deliver stem cells. The sutures were created from pig tissue, “decellularized” with detergents, to reduce the chances of inducing inflammation in…
-
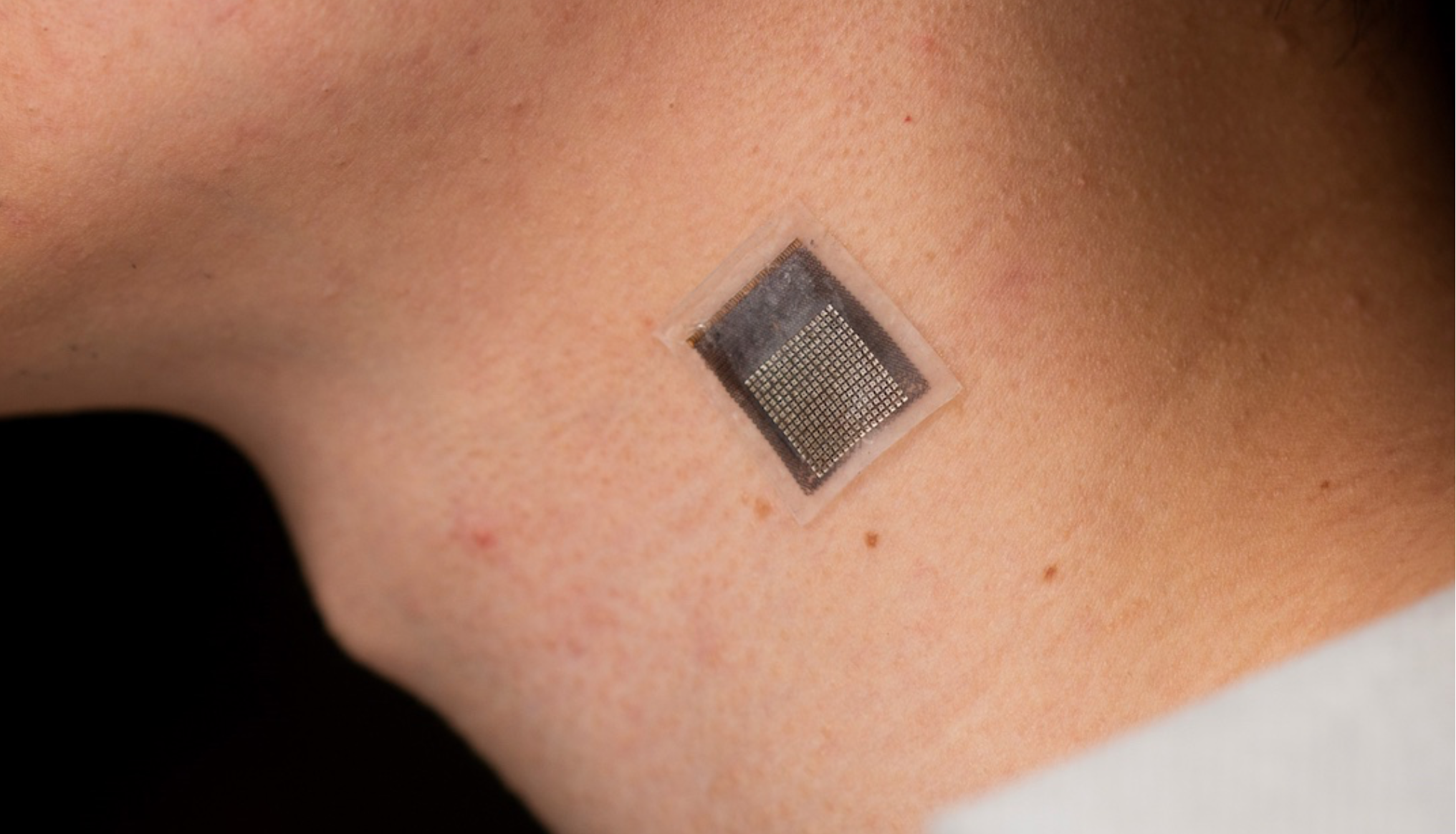
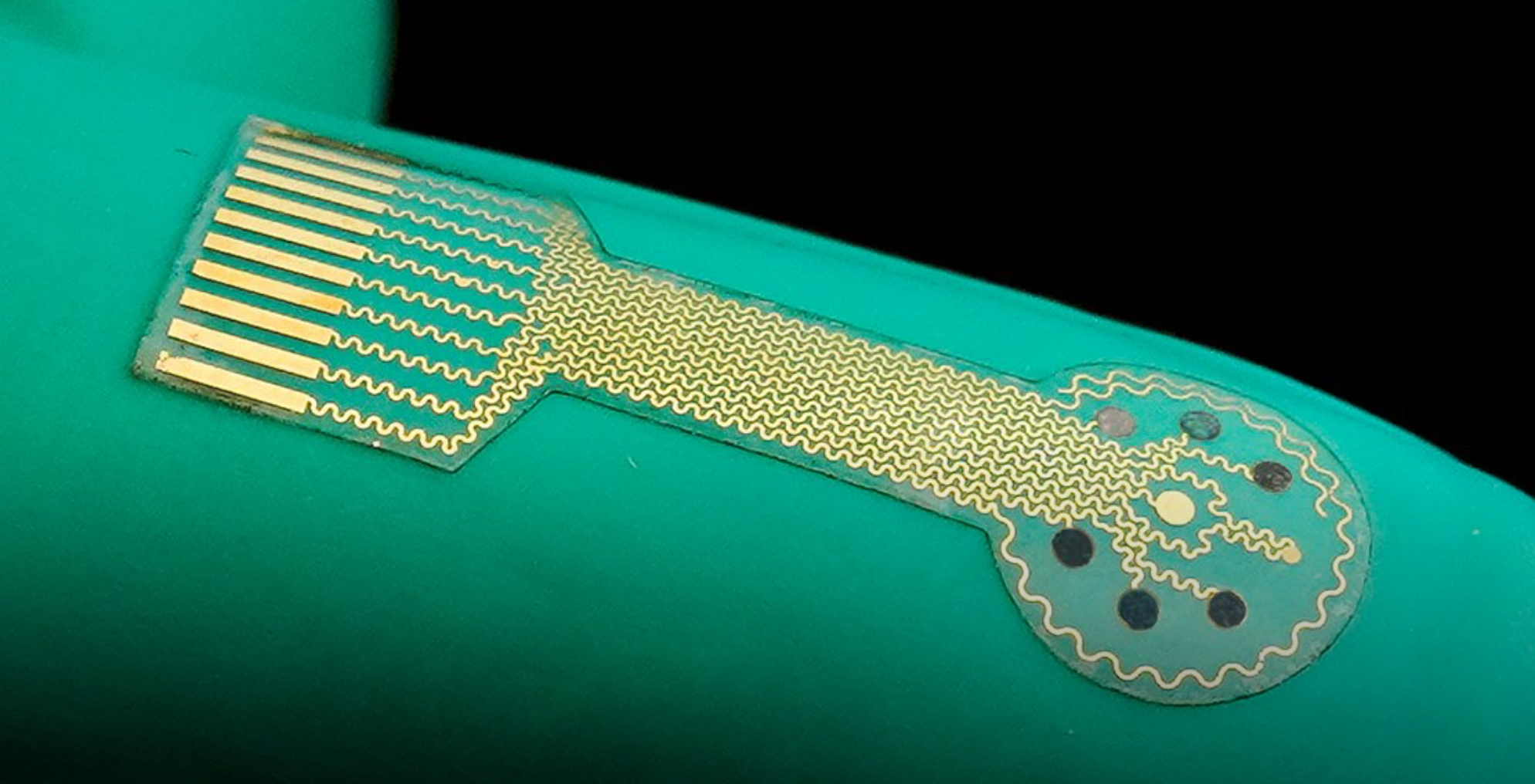
Wearable sensor evaluates human tissue stiffness
Sheng Xu and colleagues have developed a wearable, stretchable device that non-invasively evaluates the stiffness of human tissue, at an improved penetration depth, and for a longer period than, existing methods. An ultrasonic array facilitates serial, non-invasive, three-dimensional imaging of tissues, four centimeters below the surface of human skin, at a spatial resolution of 0.5…
-

Proof of concept wrist sensor could detect heart-vessel blockage in 3-5 minutes
UW’s Graham Nichol and Harborview Medical Center colleagues studying the reliability of a troponin-detecting, wrist-worn sensor in arriving cardiac arrest patients. Identifying heart-vessel blockage quickly is crucial to ensuring rapid, appropriate intervention. Traditional EKG diagnosis can lack accuracy, and blood testing for troponin can take hours. The novel “Tropsensor,” being commercialized by rce, is designed…
-
Smart bandage based closed loop wound monitoring and treatment system
Caltech professor Wei Gao has developed a smart bandage for chronic wounds, made from a flexible and stretchy polymer containing embedded electronics and medication. The electronics allow the sensor to monitor uric acid, lactate, pH level and wound temperature, indicating inflammation or bacterial infection. Data from the wound is transmitted wirelessly to the patient or…
-
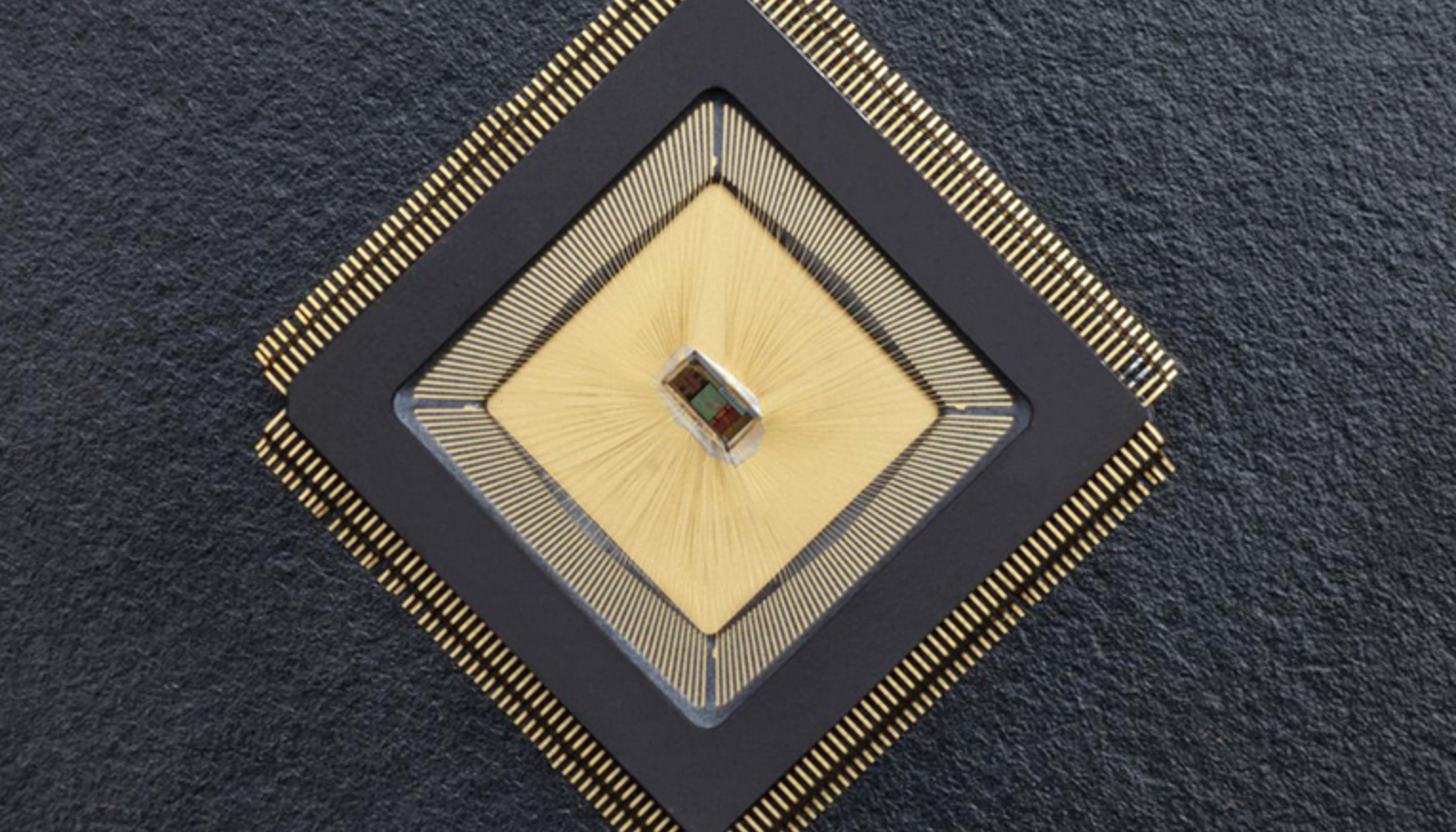
Closed-loop sensor/stimulation system to detect, reduce neurological events
For the first time, there is an autonomous sensing and stimulating unit sitting in a specific brain region and ensuring that neuronal activity in that region is controlled. The closed-loop system is called NeuralTree and was developed by Mahsa Shoaran and EPFL colleagues, to overcome the lack of control caused by epileptic activity or tremor,…
-
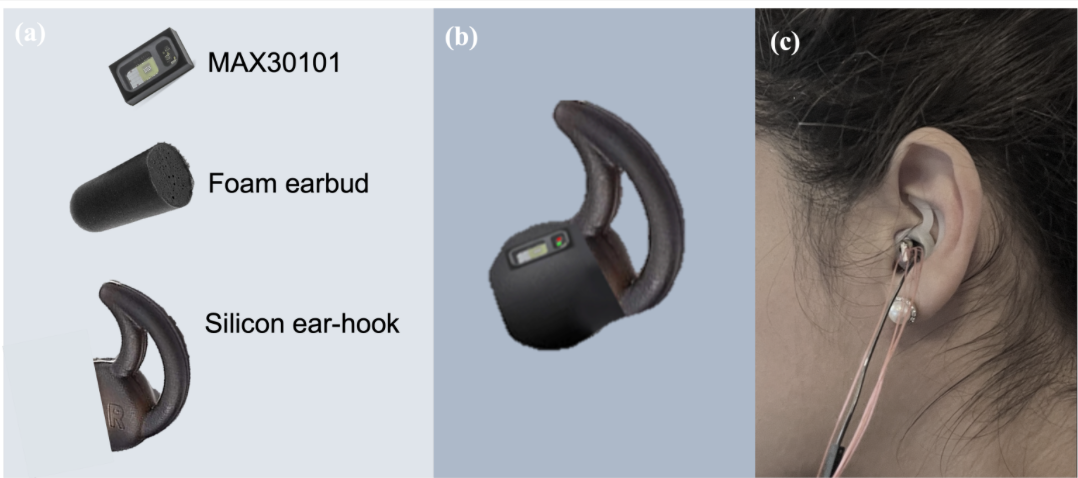
In ear PPG used to measure blood glucose levels in proof of concept study
Danilo Mandic and Imperial College colleagues have developed a novel in-ear PPG device for continuous blood glucose level measurement, using the infrared wavelength of a pulse oximeter. In a recent proof of concept study, non-diabetic, pre-diabetic, type I diabetic, and type II diabetic states were considered. Recordings spanned 9 days, in both fasting and post carbohydrate consumption…
-

Wearable sensor glows when bacteria, toxins detected
David Baker, Fiorenzo Omenetto, and University of Washington and Tufts colleagues have developed a garment-printed biopolymer sensor which detects bacteria, toxins, and dangerous chemicals. To work, a chemical activator must be sprayed after potential exposure. If the target is present, the sensor generates light. The intensity of emitted light provides a quantitative measure of the…
-
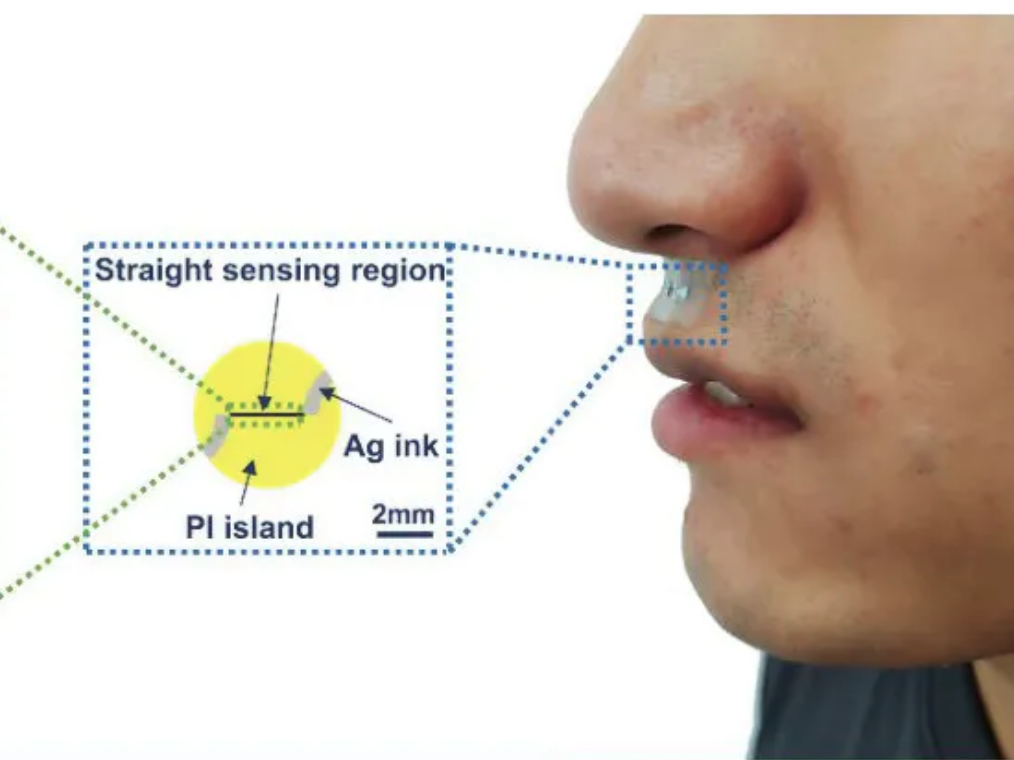
Small sticker-sensor continuously analyzes breath for broad health monitoring
Heibei University, Tianjin Hospital, Beihang University, and Penn State researchers have developed an under nose-worn, stretchable, skin-friendly, waterproof sensor to analyze breath for health monitoring. It could be use for multiple-condition screening, asthma and COPD management, or environmental hazard sensing, among other applications. The functional gas sensor, in a moisture-resistant membrane, can operate in humid…
-
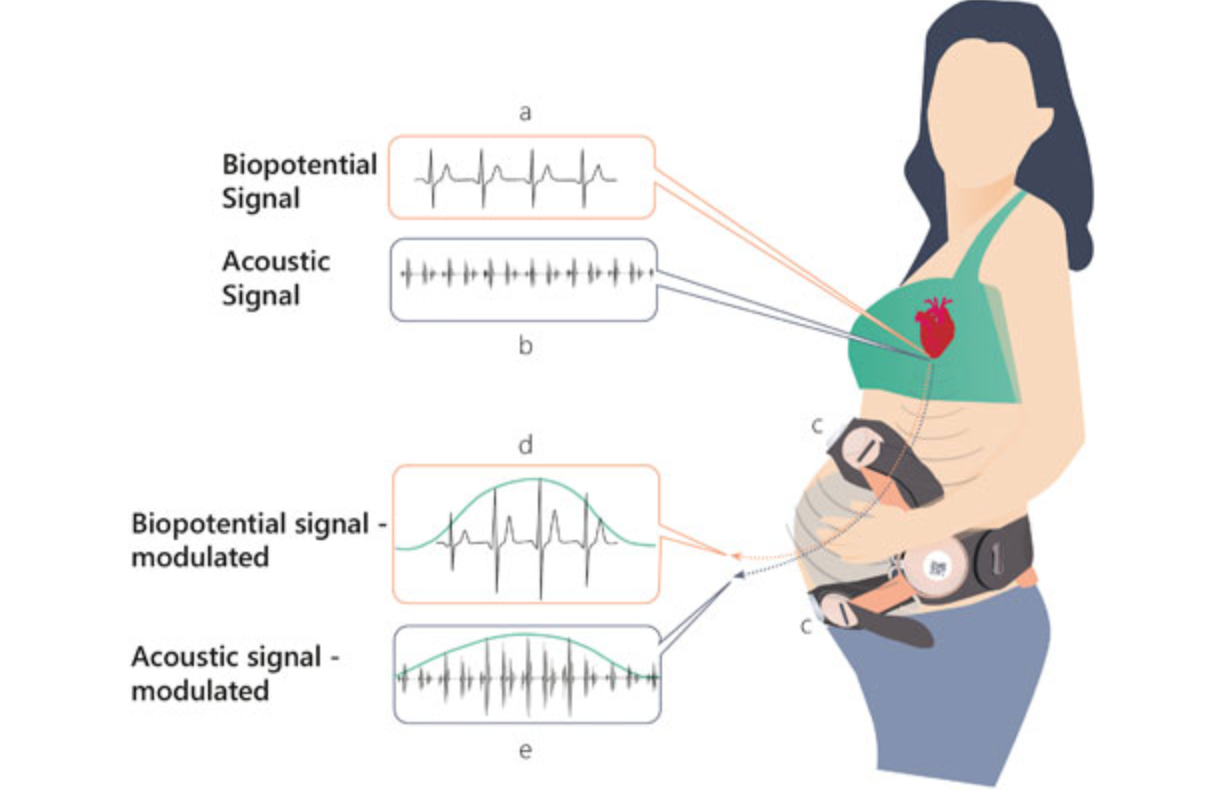
Remote, non-invasive pregnancy monitor tracks uterine activity
Uterine activity monitoring is essential to pregnancy management. Current methods are either invasive, or their accuracy is compromised by obesity, maternal movements, or belt positioning. Pregnancy-monitoring company Nuvo has published a study showing that their cardiac-derived algorithm for uterine monitoring was more accurate than TOCO standard of care in 150 patients. This remote, non-invasive detection…
-
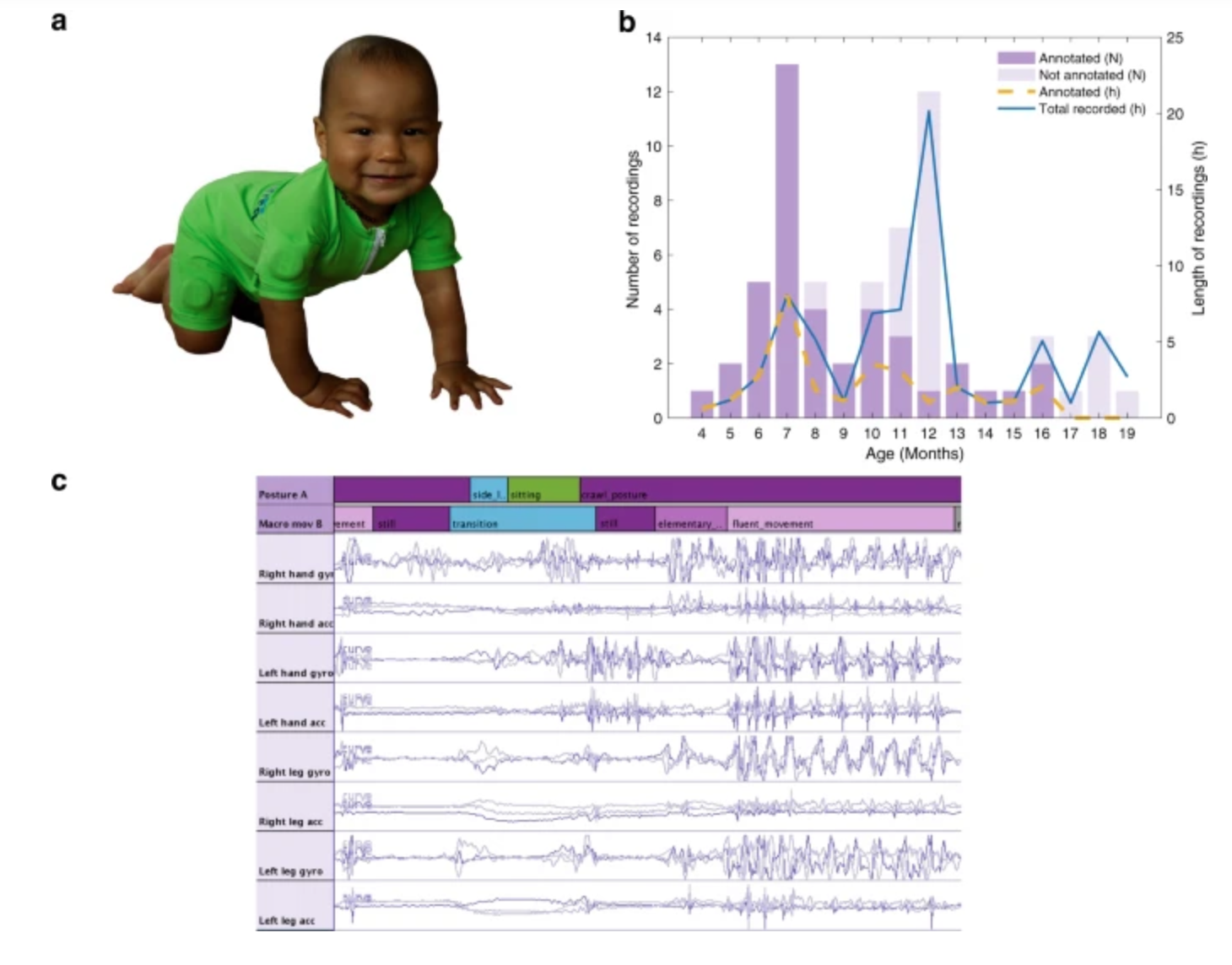
Sensor jumpsuit monitors infant motor abilities
Sampsa Vanhatalo, Manu Airaksinen and University of Helsinki colleagues have developed MAIJU (Motor Assessment of Infants with a Jumpsuit,) a wearable onesie with multiple movement sensors which they believe is able to predict a child’s neurological development. In a recent study, 5 to 19 month-old infants were monitored using MAIJU during spontaneous playtime. Initially, infant…