Category: Cancer
-
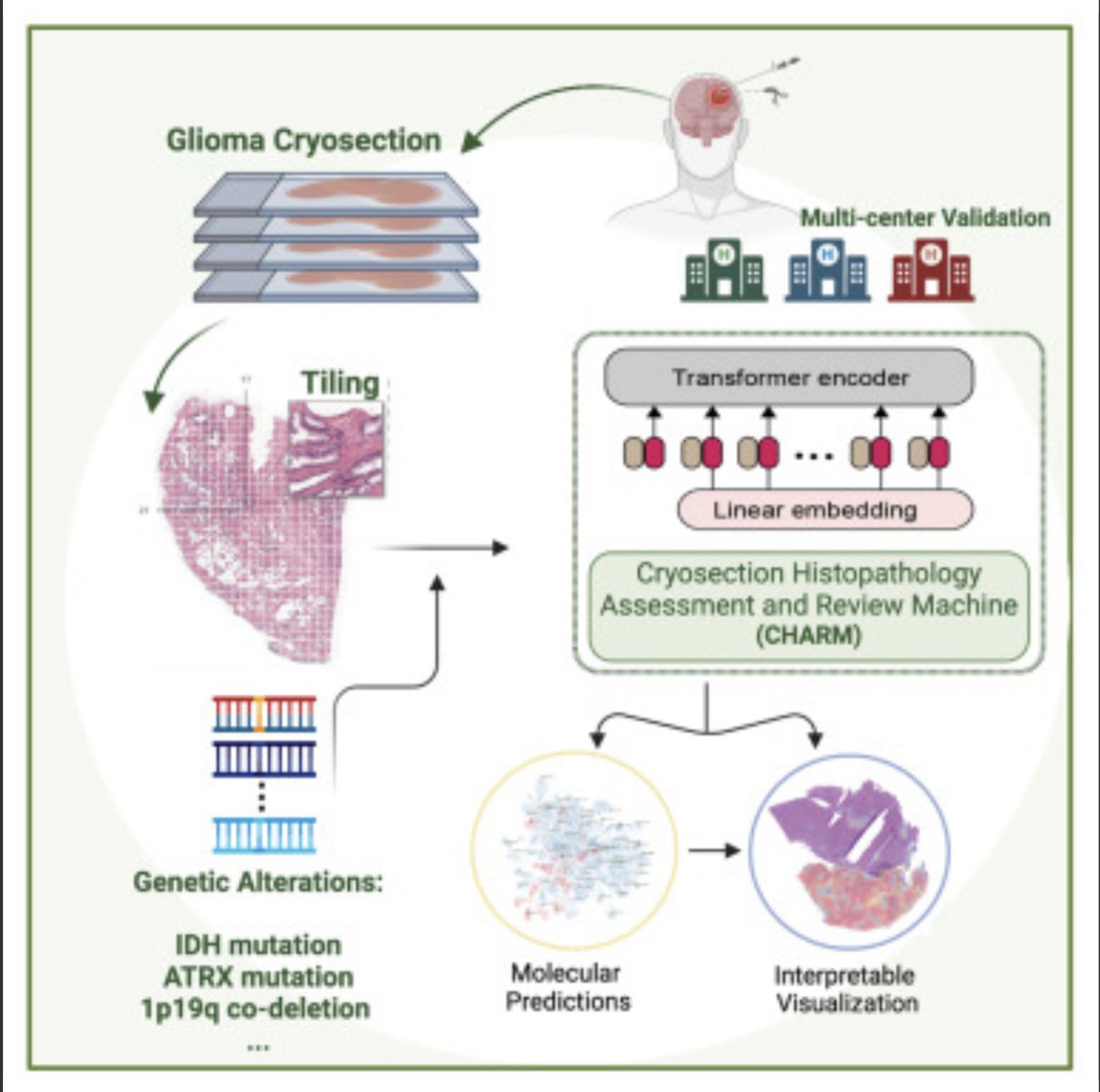
AI decodes brain tumor DNA during surgery
Kun-Hsing Yu and HMS colleagues used AI to rapidly determine a brain tumor’s molecular identity during surgery, propeling the development of precision oncology. The tool is CHARM (Cryosection Histopathology Assessment and Review Machine.) Currently, genetic sequencing takes days to weeks. Accurate molecular diagnosis during surgery can help a neurosurgeon decide how much brain tissue…
-

Wearable ultrasound to detect early breast cancer
MIT’s Canan Dagdeviren has developed a flexible ultrasound patch that can be attached to a bra, obtaining ultrasound images with resolution comparable to medical imaging centers, and used repeatedly. Interval cancers, which develop between regularly scheduled mammograms, account for 20 – 30 percent of all breast cancers, and tend to be more aggressive. The goal…
-

AI-based device increases ademona detection during colonoscopy
MAGENTIQ-COLO is an AI based FDA cleared colonoscopy device which offers a significant increase in Adenoma Detection Rate. Current high rates of missed and undetected adenomas during colonoscopy means that even regularly screened patients are still at risk of developing colon cancer. A missed polyp can lead to interval cancer, which accounts for approximately 8%…
-
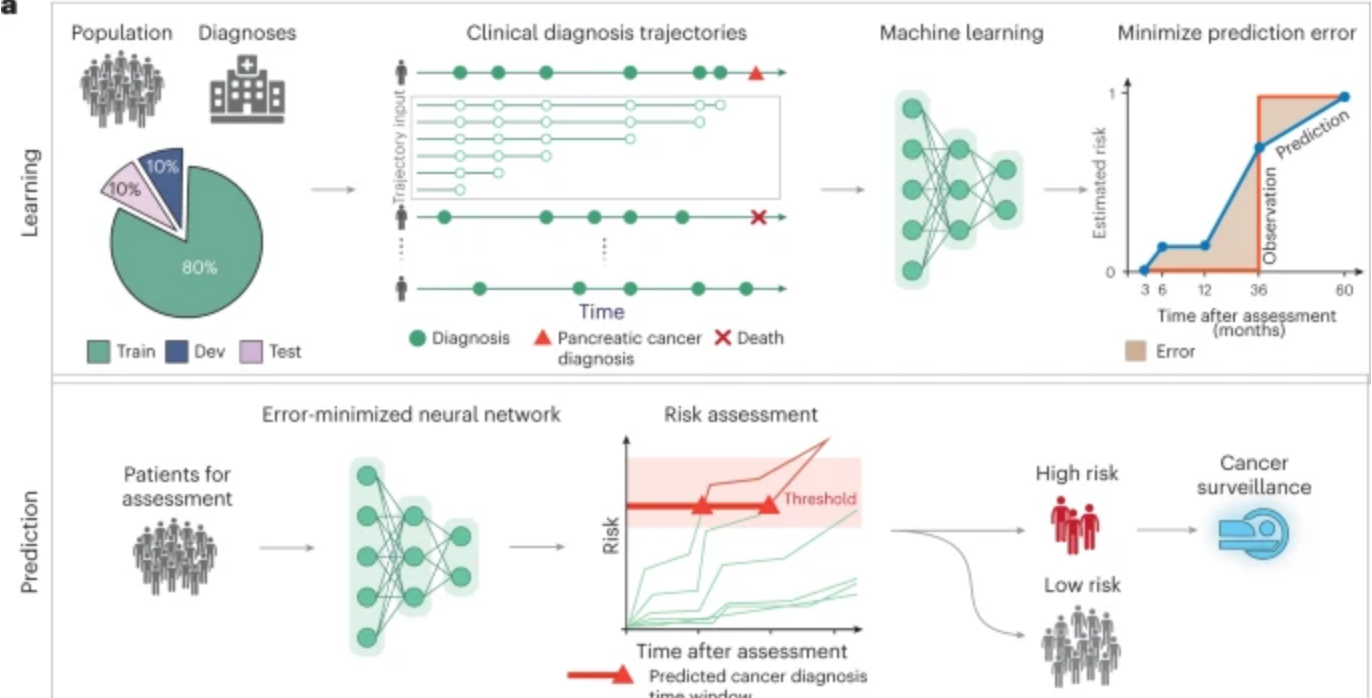
AI predicts pancreatic cancer
Harvard professor Chris Sander used clinical data from 6 million patients in Denmark’s national health system and 3 million in the U.S. VA system to train an AI model to predict the occurrence of pancreatic cancer within 3, 6, 12, and 36 months. This could allow wider screening for the aggressive disease, which is often…
-
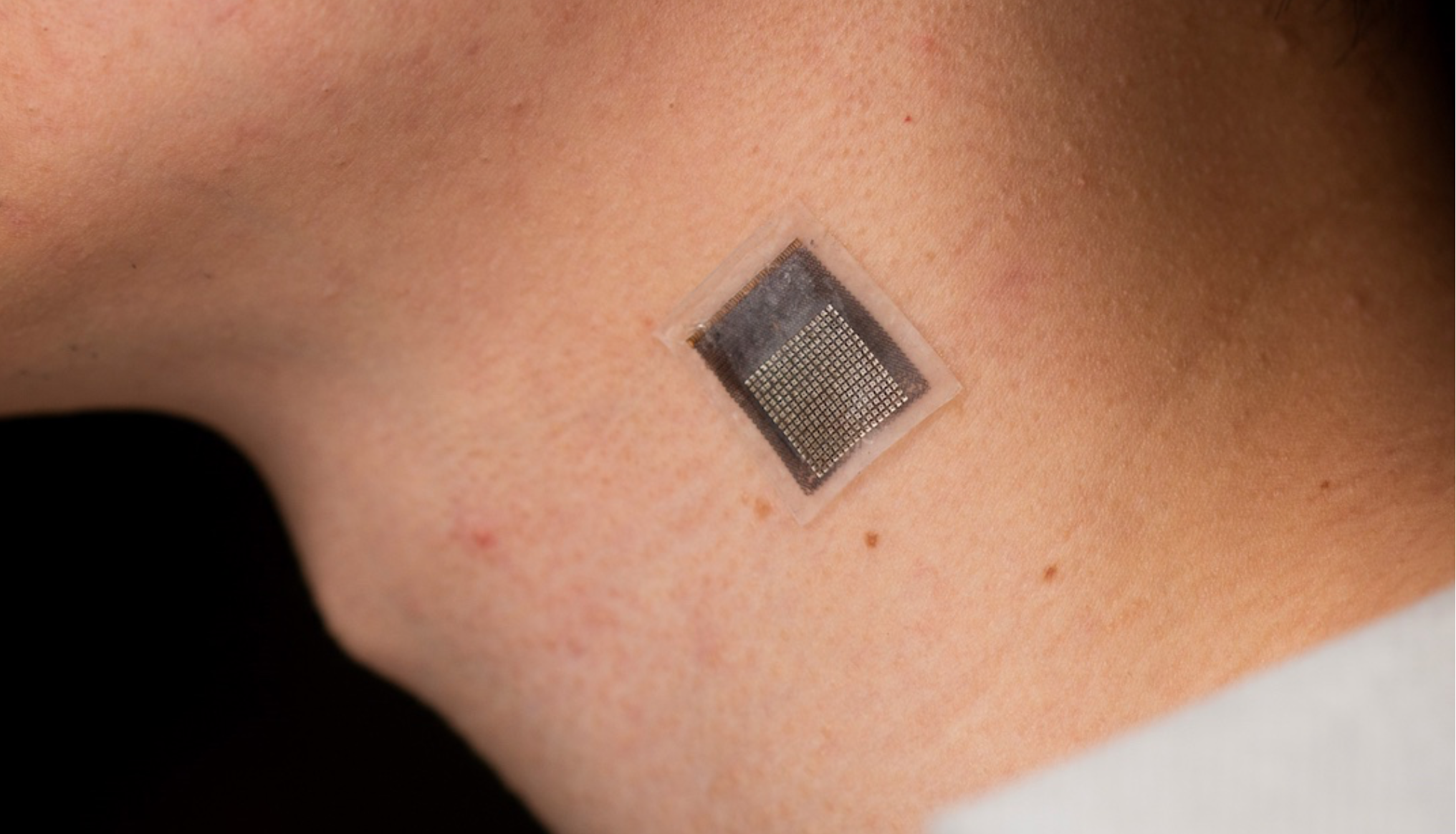
Wearable sensor evaluates human tissue stiffness
Sheng Xu and colleagues have developed a wearable, stretchable device that non-invasively evaluates the stiffness of human tissue, at an improved penetration depth, and for a longer period than, existing methods. An ultrasonic array facilitates serial, non-invasive, three-dimensional imaging of tissues, four centimeters below the surface of human skin, at a spatial resolution of 0.5…
-
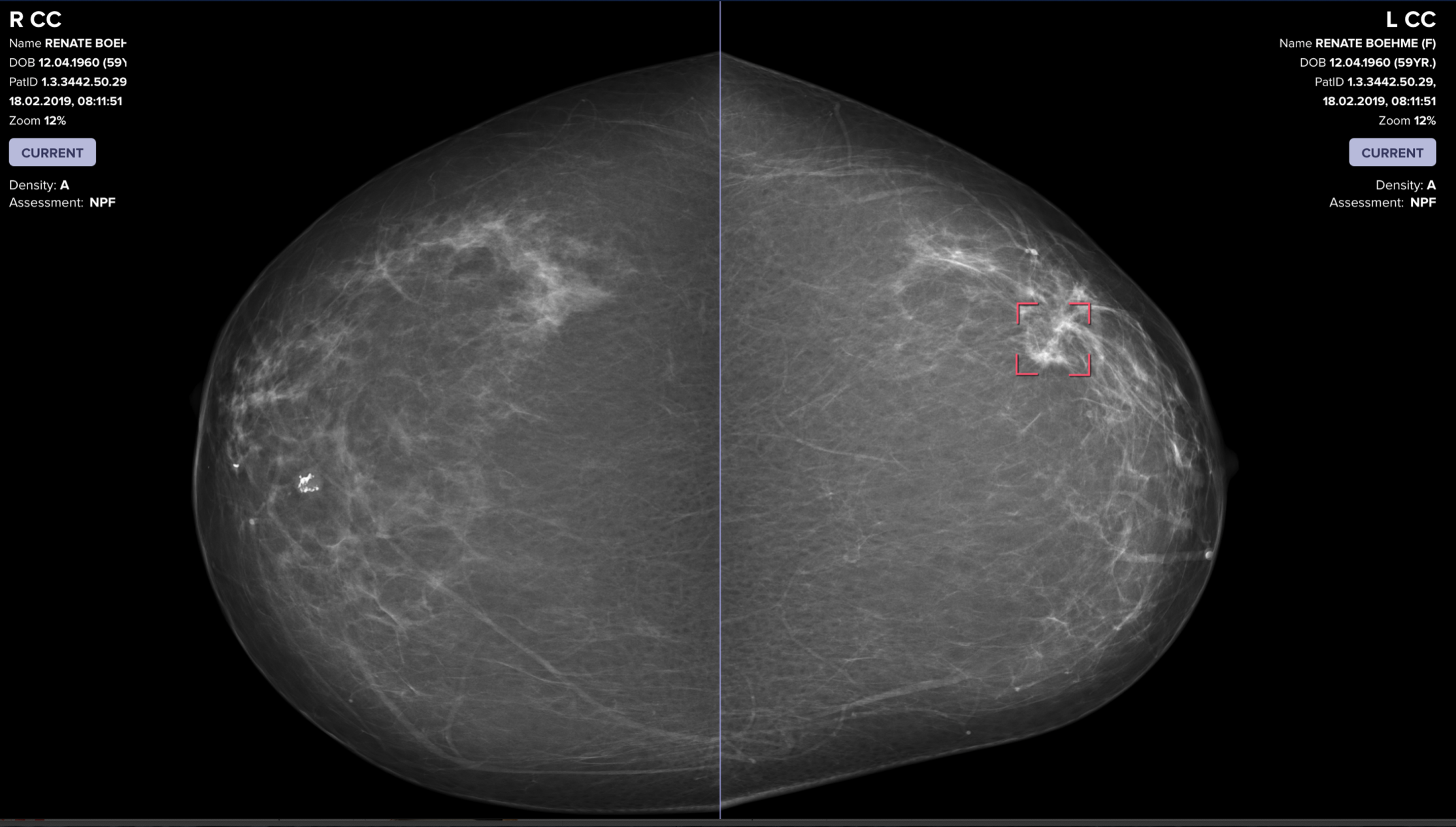
AI catches breast cancer earlier, more often than traditional screening alone
The mammography screening paradigm has not changed since the 1960s. Breast screening AI company Vara, with Essen University and Memorial Sloan Kettering hospitals, published a study showing that radiologists assisted by AI are better able to screen for breast cancer. The hope is that AI systems could detect cancers that doctors miss, provide better care…
-
MSK developed sensor detects molecular signature of cancer; compared to human scent
Mijin Kim and Daniel Heller of the Nanomedicine Lab at Memorial Sloan Kettering Cancer Center have developed an array of carbon nanotube sensors that can “sniff” cancer using AI. The human nose can detect a trillion different scents, through hundreds of olfactory receptors. The pattern which odor molecules bind to which receptors creates a kind…
-

AI for (much) earlier breast cancer detection – Constance Lehman
Connie Lehman — Professor, Radiology, Harvard Medical School; Chief of Breast Imaging, radiology, Massachusetts General Hospital; Co-director of AVON Breast Center, Radiology, Massachusetts General Hospital; and Director, Breast Imaging Research Center, Radiology, Massachusetts General Hospital spoke at ApplySci’s recent conference at Harvard Medical School. Click to listen to her talk on using AI to discover breast cancer 5 years…
-
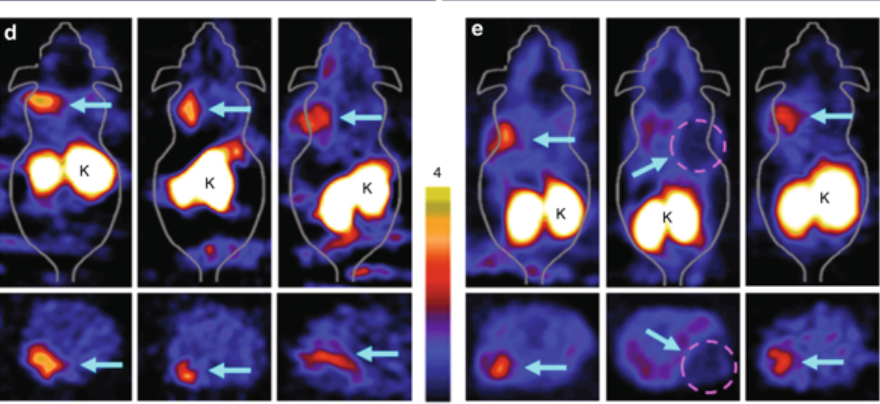
PET scan tracer detects both cancer and lung disease
Stanford’s Sanjiv Gambhir has developed an imaging molecule that can identify pancreatic, cervical and lung cancer early– and, surprisigly, hard-to-detect idiopathic pulmonary fibrosis. The tracer clings to integrin alpha-v beta-6. In a PET scan, the tracer glows due to radioactivity emissions, which allows doctors to see exactly where the tracer is docked in the body. A…
-
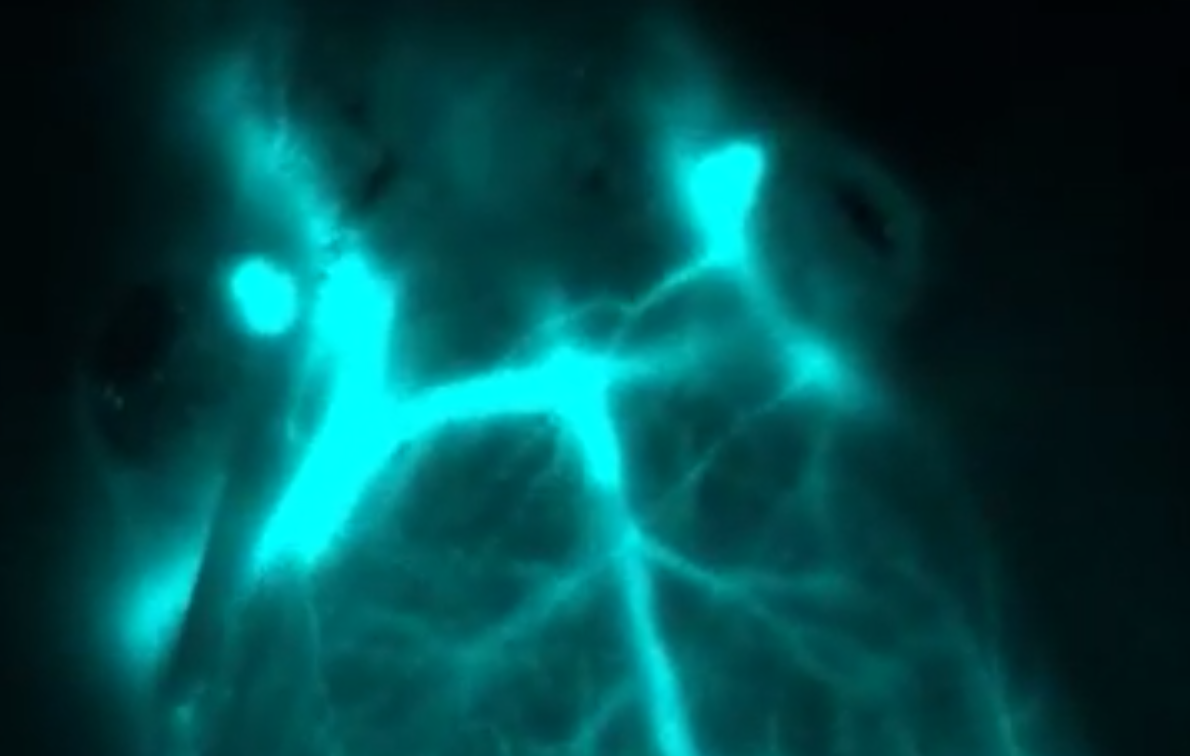
Infrared light detects tumors under the skin
Stanford’s Hongjie Dai has developed a deep-tissue imaging technique that clearly illuminates tumors beneath the skin. It relies on nanoparticles containing erbium, which glows in the infrared. The promising technology has only been tested on mice, so far. In a study, the technique was used to predict cancer patient response to immunotherapy, and to measure drug…
-
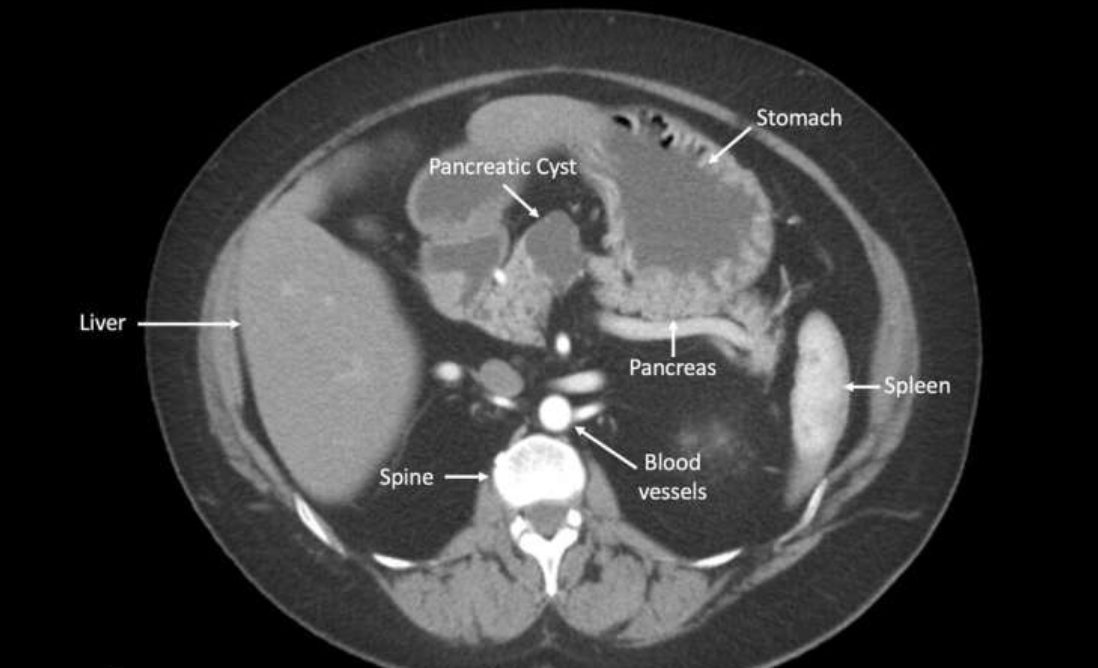
AIgorithm detects cancer potential of pancreatic cysts
CompCyst is a proof-of-concept study, led by Anne Marie Lennon at Johns Hopkins, which uses AI to more accurately determine which pancreatic cysts will become cancerous. The test evaluates molecular and clinical markers in cyst fluids, and could significantly improve detection rates vs. current clinical and imaging tests. In the study, the researchers evaluated molecular profiles,…
-
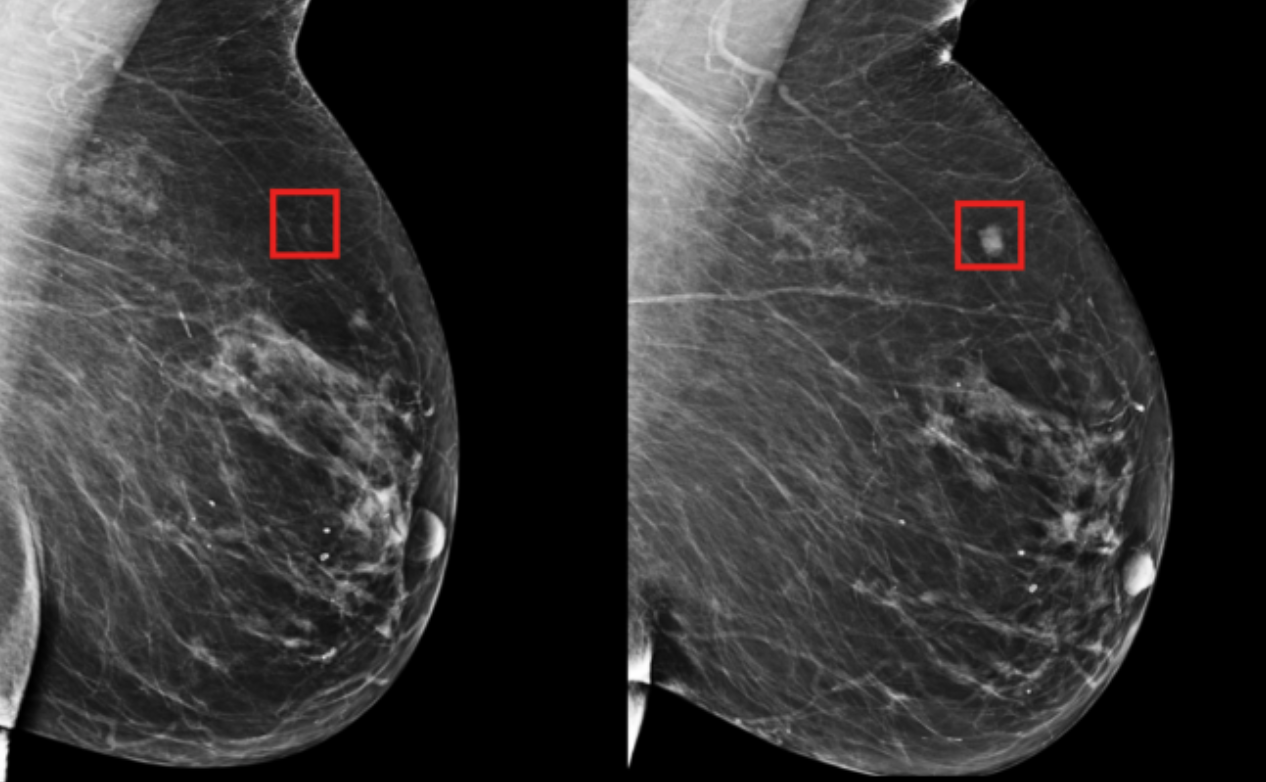
Deep learning mammography model detects breast cancer up to five years in advance
MIT CSAIL professor Regina Barzilay and Harvard/MGH professor Constance Lehman have developed a deep learning model that can predict breast cancer, from a mammogram, up to five years in the future. The model learned subtle breast tissue patterns that lead to malignant tumors from mammograms and known outcomes of 90,000 MGH patients. The goal is…