Category: Stem Cells
-
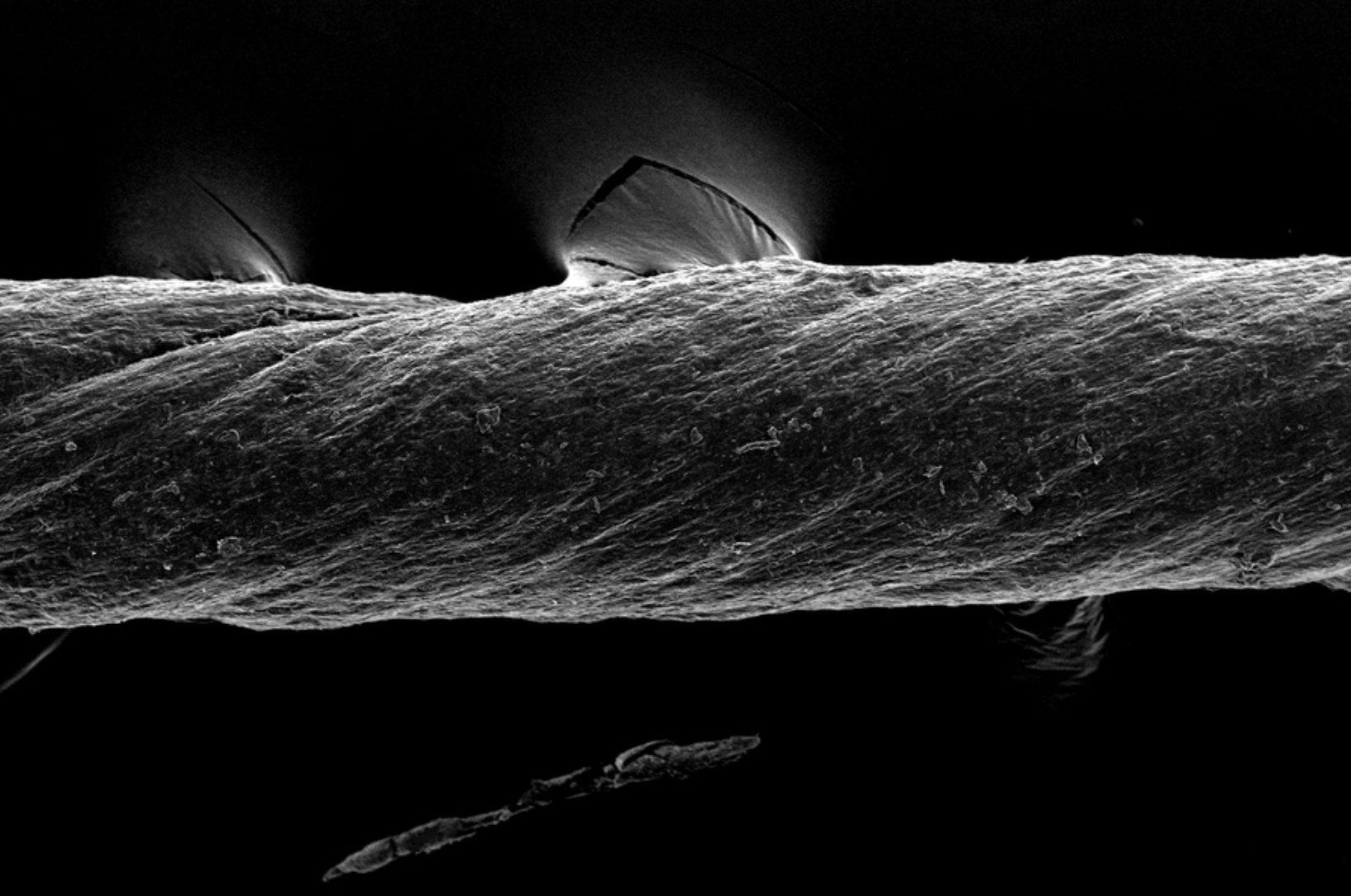
Hydrogel-coated sutures sense inflammation, can deliver drugs and stem cells
Giovanni Traverso has designed tough, absorbable, hydrogel-coated sutures, which in addition to holding post-surgery or wound-affected tissue in place, can sense inflammation and deliver drugs, including monoclonal antibodies. They could also be used to deliver stem cells. The sutures were created from pig tissue, “decellularized” with detergents, to reduce the chances of inducing inflammation in…
-

Stem cell treatment for ARDS in COVID-19 patients
Last week, Pluristem released initial results from its compassionate use program for the treatment of patients with acute respiratory failure and inflammatory complications resulting from COVID-19. The treatment was administered in an Israeli hospital. All seven ICU patients with ARDS treated with Pluristem’s PLX cell therapy have survived. 6 out of 7 have completed the…
-
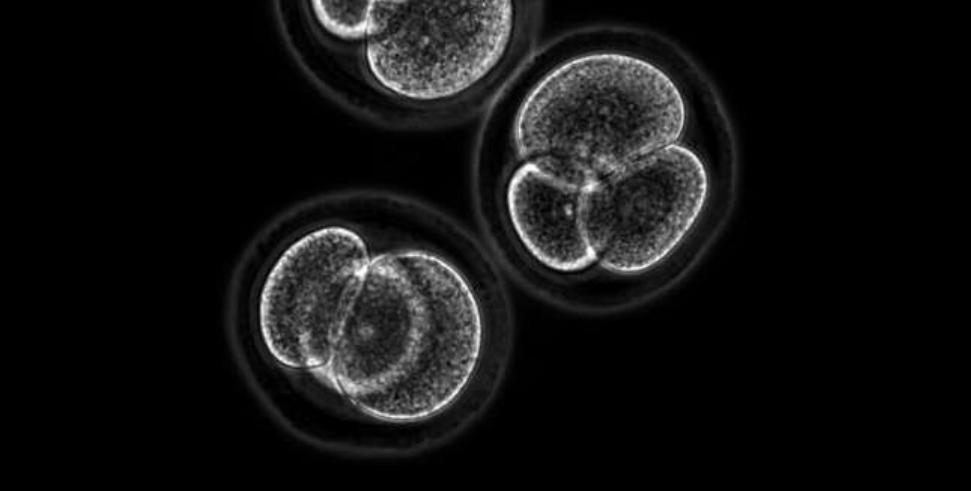
Embryo stem cells created from skin cells
Yossi Buganim from The Hebrew University of Jerusalem has discovered a set of genes that can transform murine skin cells into all three of the cell types that comprise the early embryo: the embryo itself, the placenta and the extra-embryonic tissues, such as the umbilical cord. Buganim and colleagues discovered a combination of five genes…
-
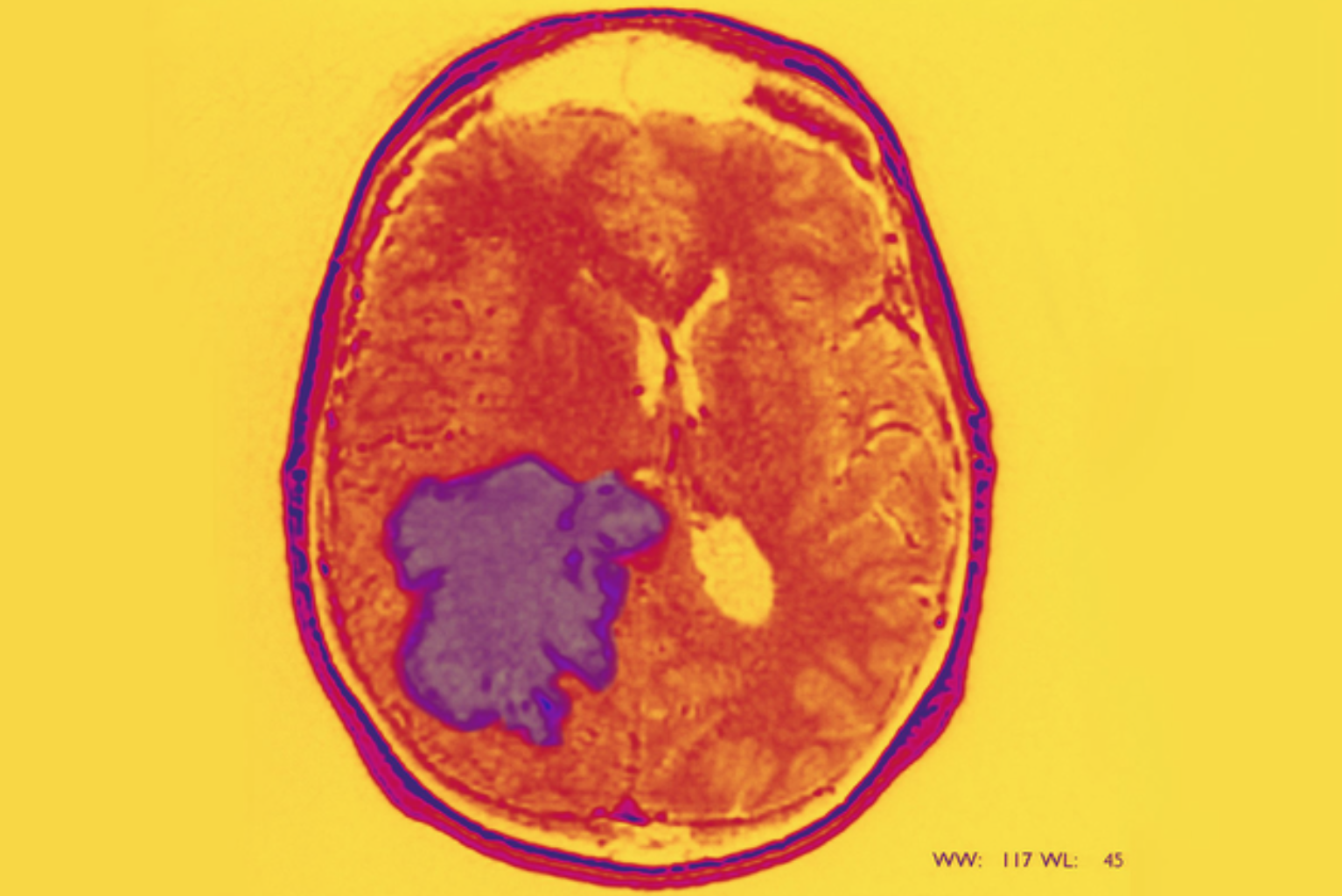
Starving cancer stem cells as a new approach to glioblastoma
Luis Parada and Sloan Kettering colleagues are focusing on cancer stem cells as a new approach to glioblastoma. Like normal stem cells, cancer stem cells have the ability to rebuild a tumor, even after most of it has been removed, leading to cancer relapse and metastasis. According to Parada: “The pharmaceutical industry has traditionally used…
-
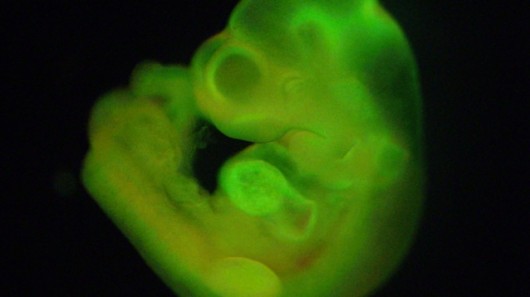
Nobel-worthy stem cell discovery
http://www.nature.com/news/acid-bath-offers-easy-path-to-stem-cells-1.14600 Haruko Obokata and colleagues at the RIKEN Center for Developmental Biology have created embryonic stem cells from a single blood cell by putting white blood cells from a baby mouse in a mild acid solution. Eventually a few stem cells emerge that can turn into any other cell in the body including skin, heart, liver or neurons.…