Tag: Sensor
-
Carbon nanotube sensor precisely measures dopamine
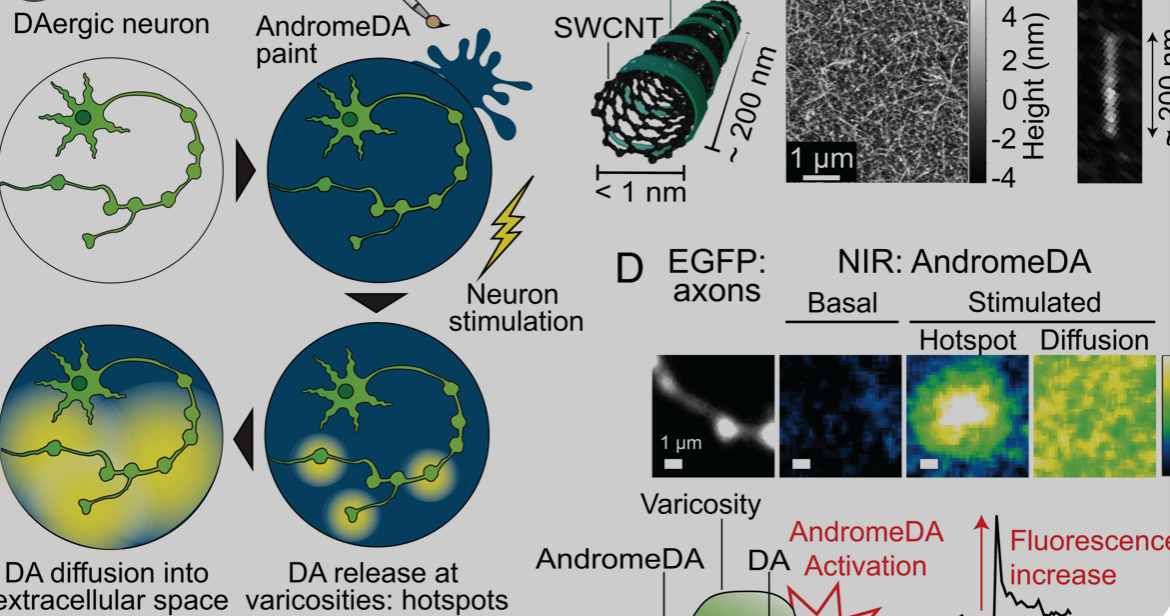
Ruhr University professor Sebastian Kruss, with Max Planck researchers Sofia Elizarova and James Daniel, has developed a sensor that can visualize the release of dopamine from nerve cells with unprecedented resolution. The team used modified carbon nanotubes that glow brighter in the presence of the messenger substance dopamine. Eizarova said that the sensor “provides new…
-
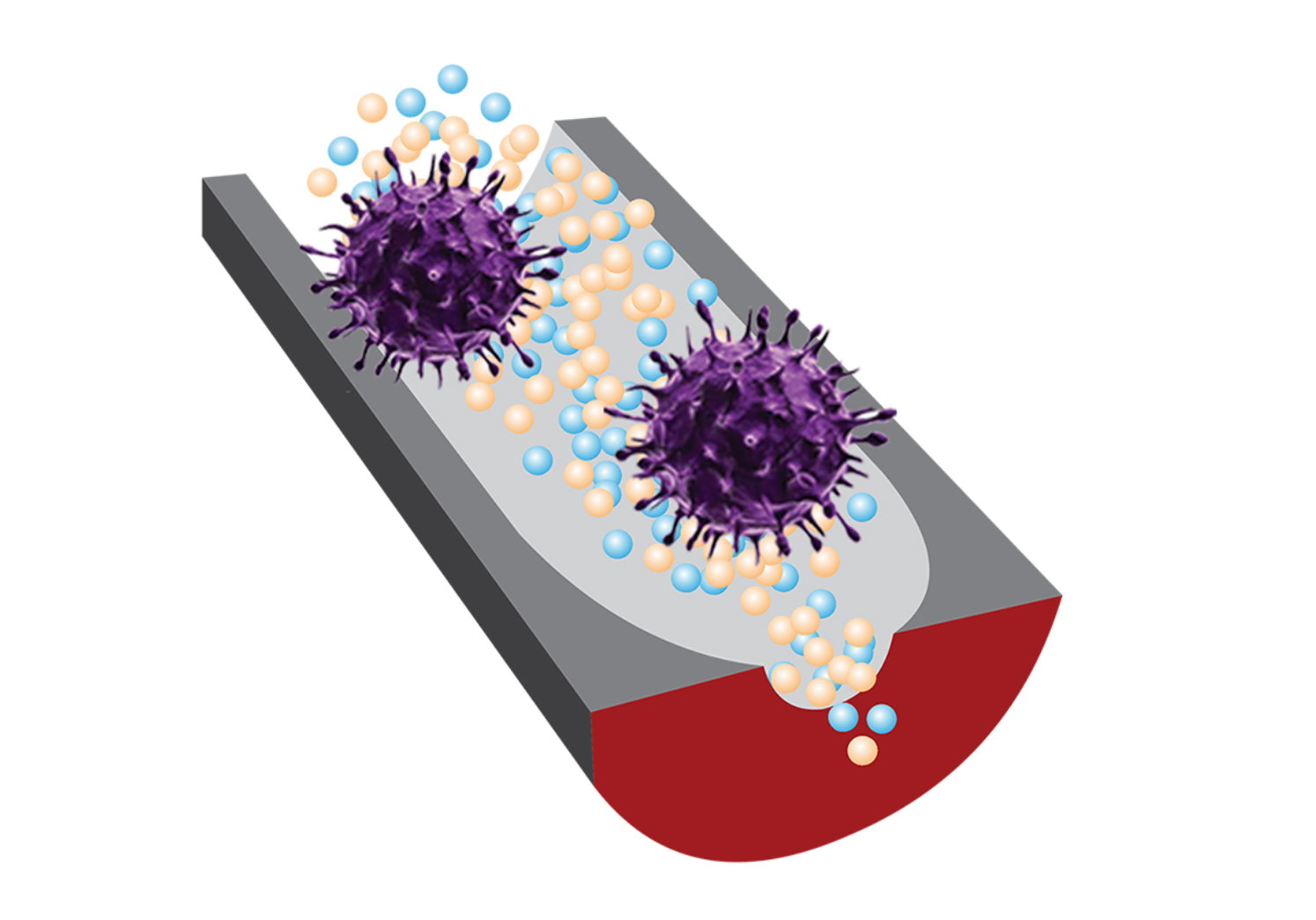
DNA sensor detects whether virus is present and infectious, including COVID 19
Yi Lu and Benito Marinas at the University of Illinois and University of Texas have developed a sensor that detects both the presence of a virus and whether or not it is infectious, integrating purpose designed DNA fragments and nanopore sensing. They have already studied its potential with the adenovirus and COVID 19. Current PCR…
-

Sweat sensor monitors drug levels, informs dosage
Sam Emaminejad, Shuyu Lin, Carlos Milla, Ronald Davis and UCLA and Stanford colleagues have developed a watch which monitors drug levels inside the body by analyzing a wearer’s sweat. The goal is individually tailored drug dosages. Dosages are currently prescribed based on statistical effectiveness averages driven by weight and age. However, constantly changing body chemistry…
-
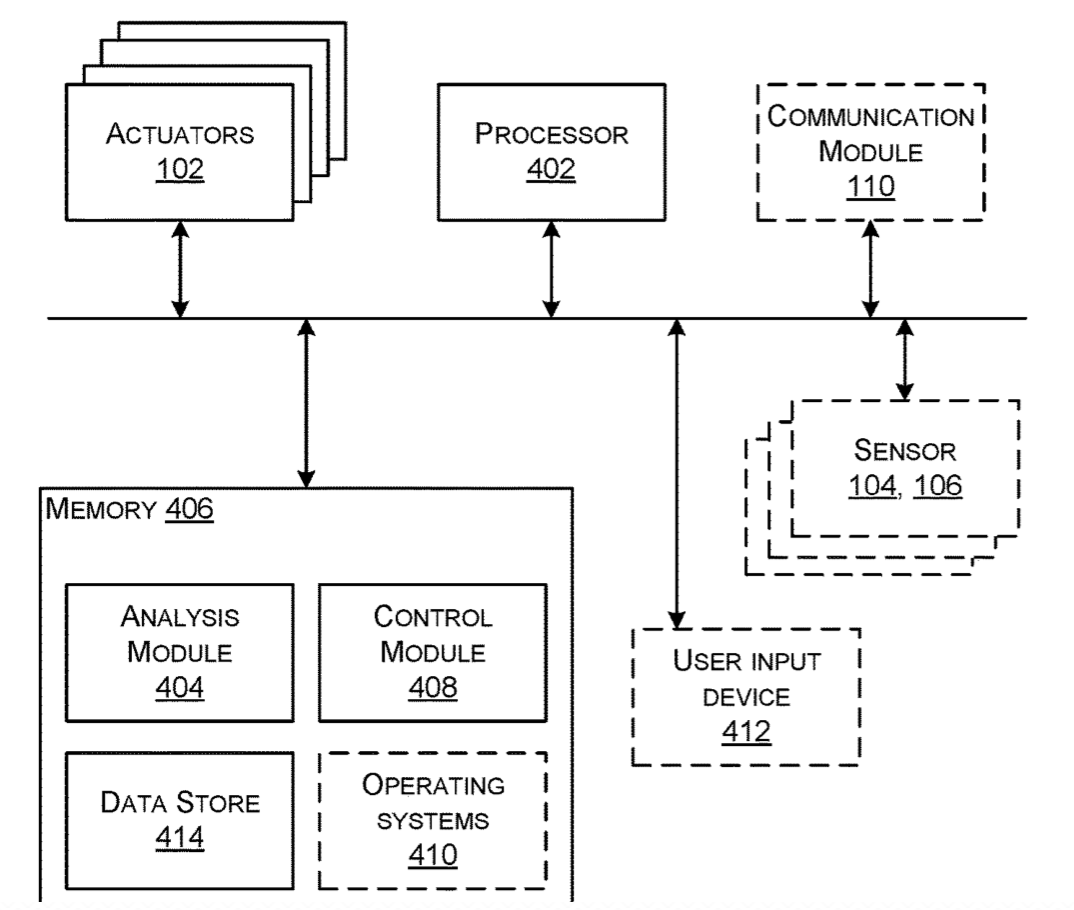
Wearable haptic feedback/stimulation band to address Parkinson’s symptoms
Microsoft has submitted a patent application for a wearable band that uses haptic feedback for stimulation when wrapped around limbs or joints. It is meant to alleviate Parkinson’s symptoms, including tremors and muscle stiffness. Haptic actuators are distributed across a band that is adjusted to a “duty cycle” which responds to data derived from wearable…
-

Wearable sensor monitors shunt function in hydrocephalus
Northwestern’s John Rogers has created another minimal, flexible, wireless, adhesive wearable — this time to help hydrocephalus patients manage their condition. The band-aid like sensor determines whether a shunt is working properly. Shunts often fail. When this happens, a patient can experience headaches, nausea and low energy, and must go to a hospital immediately. However,…
-
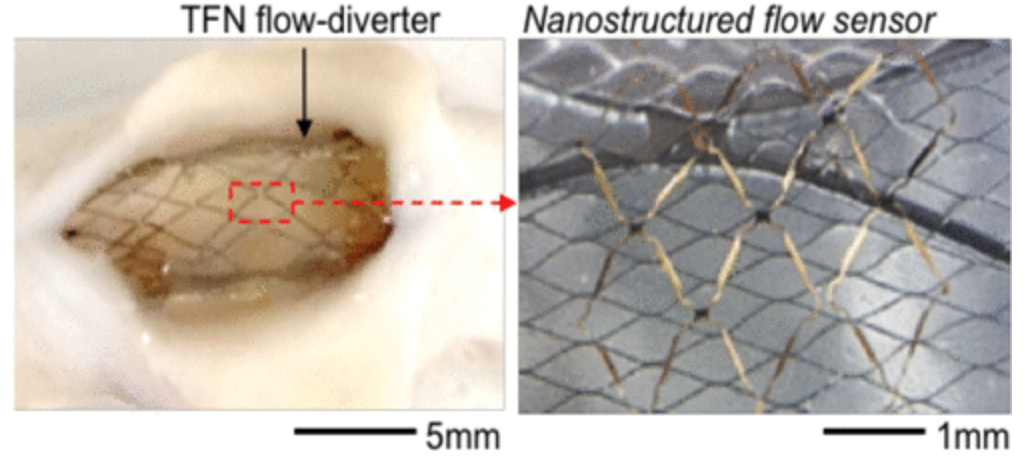
Sensor could continuously monitor brain aneurysm treatment
Georgia Tech’s Woon-Hong Yeo has developed a proof of concept, flexible, stretchable sensor that can continuously monitor hemodynamics when integrated with a stent like flow diverter after a brain aneurysm. Blood flow is measured using capacitance changes. According to Pittsburgh professor Youngjae Chun, who collaborated with Yeo, “We have developed a highly stretchable, hyper-elastic flow diverter using a…