Category: Parkinson’s
-
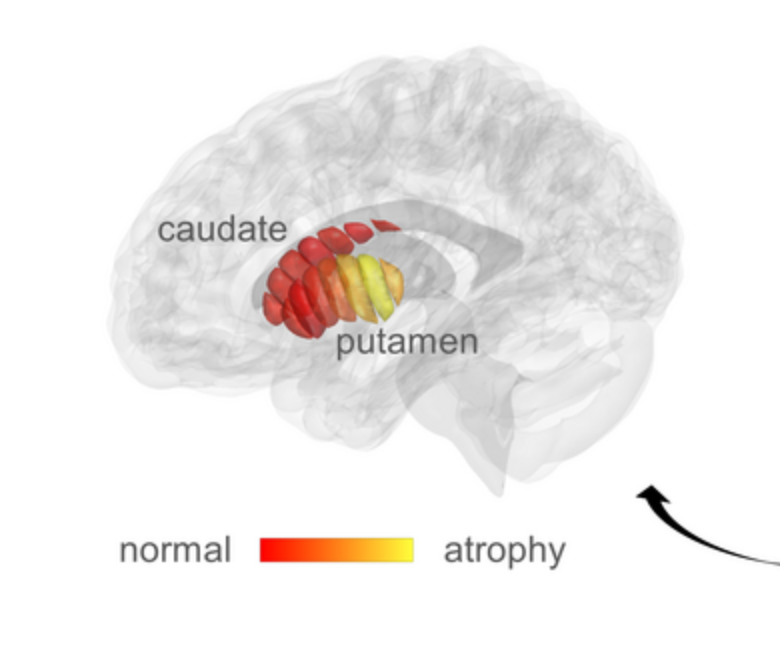
qMRI for early detection of Parkinson’s disease
Aviv Mezer and Hebrew University colleagues used quantitative MRI to identify cellular changes in Parkinson’s disease. Their method enabled them to look at microstructures in the striatum, which is known to deteriorate during disease progression. Using a novel algorithm developed by Elior Drori, biological changes in the striatum were revealed, and associated with early stage…
-

Neural Network assesses sleep patterns for passive Parkinson’s diagnosis
MIT’s Dina Katabi has developed a non-contact, neural network-based system to detect Parkinson’s disease while a person is sleeping. By assessing nocturnal breathing patterns, the series of algorithms detects, and tracks the progression of, the disease — every night, at home. A device in the bedroom emits radio signals, analyzes their reflections off the surrounding…
-
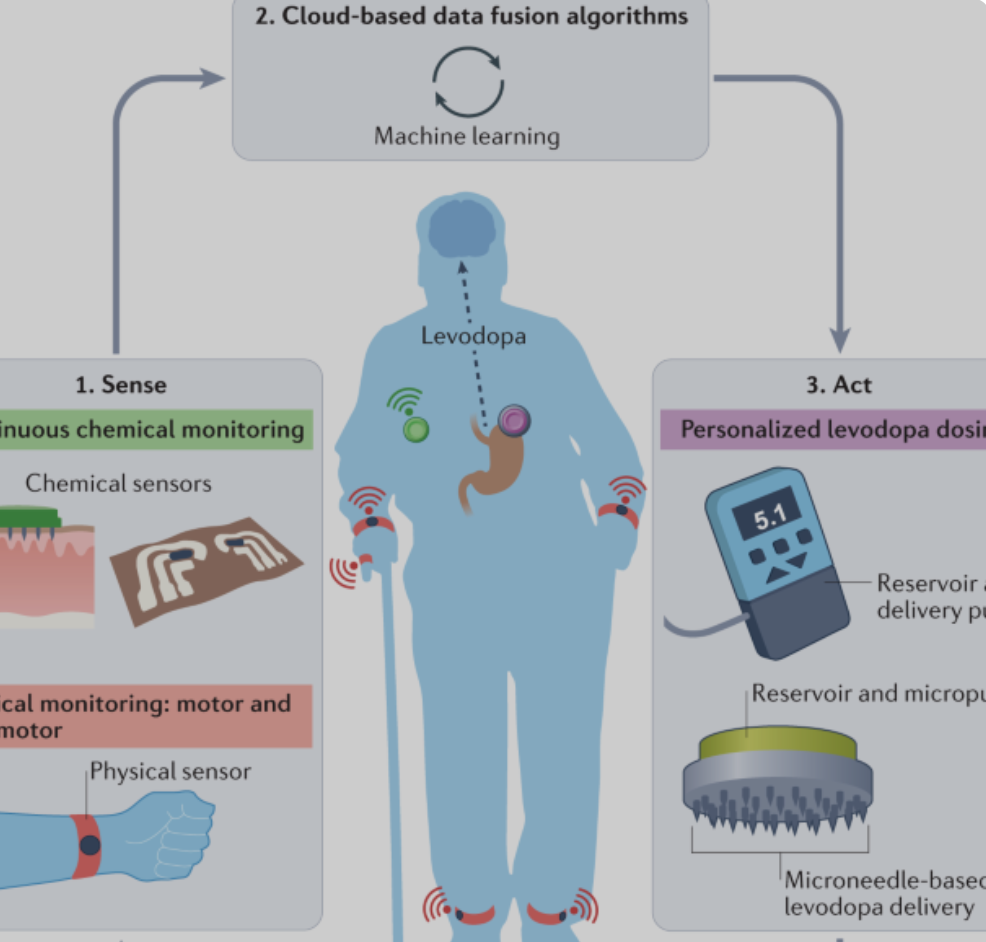
Joe Wang developed, closed-loop, levadopa delivery/monitoring system for Parkinson’s disease
Early Parkinson’s Disease patients benefit significantly from levodopa, to replace dopamine to restore normal motor function. As PD progresses, the brain loses more dopamine-producing cells, which causes motor complications and unpredictable responses to levodopa. Doses must be increased over time, and given at shorter intervals. Regimens are different for each person and may vary from…
-

Directional DBS system targets GPi to relieve Parkinson’s symptoms
Abbott received FDA approval for an expanded indication for its Deep Brain Stimulation system, to include targeting of internal globus pallidus. The GPi plays an integral role in motor function. When targeted with DBS, Parkonson’s symptoms not adequately controlled by medication can improve. The directed stimulation system is now approved for all major targets used…
-
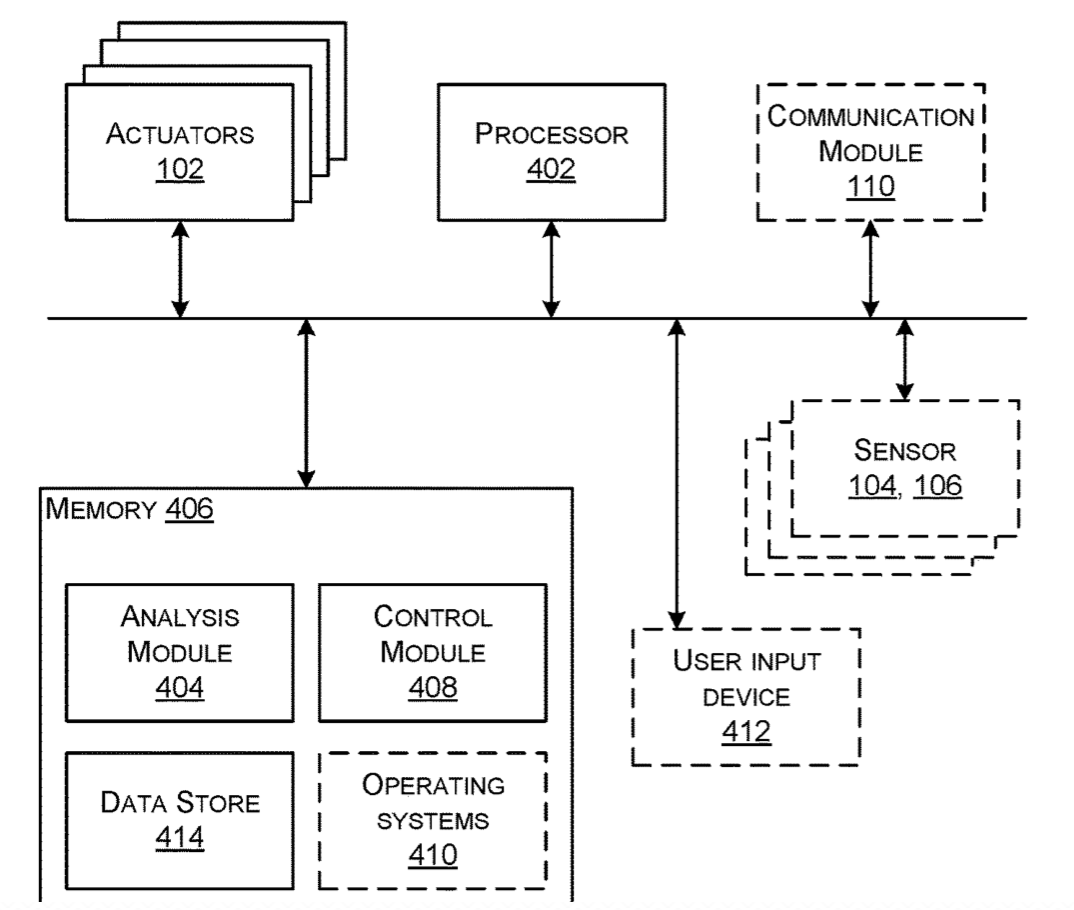
Wearable haptic feedback/stimulation band to address Parkinson’s symptoms
Microsoft has submitted a patent application for a wearable band that uses haptic feedback for stimulation when wrapped around limbs or joints. It is meant to alleviate Parkinson’s symptoms, including tremors and muscle stiffness. Haptic actuators are distributed across a band that is adjusted to a “duty cycle” which responds to data derived from wearable…
-
Focused ultrasound thalamotomy in Parkinson’s Disease
UVA’s Scott Sperling and Jeff Elias, who already used focused ultrasound to treat essential tremor, have just published the results of a small study showing the efficacy of the technology in Parkinson’s Disease. The sound waves were shown to interrupt brain circuits responsible for the uncontrollable shaking associated with the disease. The researchers claim that their study…
-
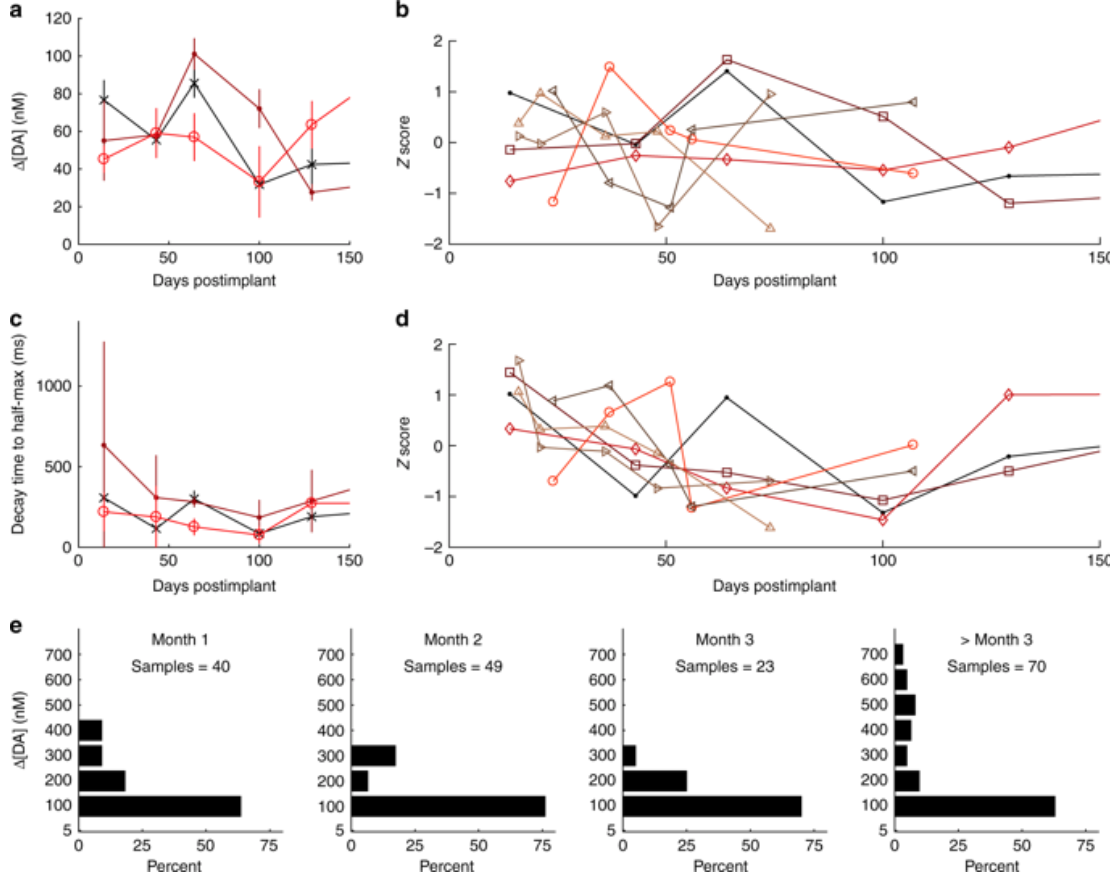
Implanted sensors track dopamine for a year
Helen Schwerdt, Ann Graybiel, Michael Cima, Bob Langer, and MIT colleagues have developed and implantable sensor that can measure dopamine in the brain of rodents for more than one year. They believe that this can inform the treatment and understanding of Parkinson’s and other brain diseases. According to Graybiel, “Despite all that is known about…
-

AI driven, music-triggered brain state therapy for pain, sleep, stress, gait
The Sync Project has developed a novel, music-based, non-pharmaceutical approach to treating pain, sleep, stress, and Parkinson’s gait issues. Recent studies showed Parkinson’s patients improved their gait when listening to a song with the right beat pattern, and post surgery patients used 1/3 the amount of self-administered morphine after listening to an hour of music.…
-

Verily’s health sensing research watch
The Verily Study Watch passively captures health data for continuous care platforms and clinical research. Key features described by the company include: Multiple physiological and environmental sensors are designed to measure relevant signals for studies spanning cardiovascular, movement disorders, and other areas. Examples include electrocardiogram (ECG), heart rate, electrodermal activity, and inertial movements. A long…
-

VR training to reduce falls in Parkinson’s, dementia
Tel Aviv University’s Jeff Hausdorff has created a virtual reality treadmill system in an attempt to prevent falls in Parkinson’s and dementia patients. Current interventions focus on improving muscle strength, balance and gait. By integrating motor planning, attention, executive control and judgement training, using VR, therapies can also address the cognitive issues associated with falls. In…
-
Carbon electrode technique tracks dopamine in the brain
Michael Cima and MIT colleagues have developed a more precise tool to measure dopamine in the brain, to be able to study its role in in learning, memory, and emotion. The new carbon electrode based technique can cover more of the brain, and provide longer, more accurate neurotransmitter readings, than previously possible. The goal is…
-
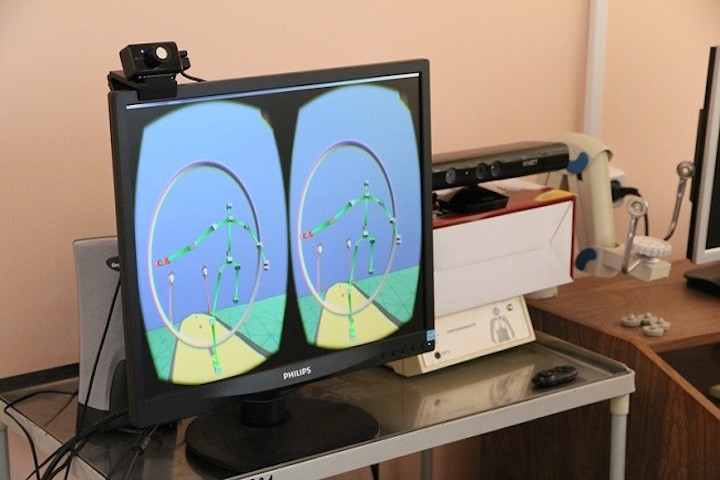
VR for early neurodegenerative disease detection, personalized rehabilitation
Tomsk Polytechnic and Siberian State University scientists David Khachaturyan and Ivan Tolmachov have developed a VR based neurodegenerative disorder diagnosis system. The goal is the early detection and tretment of diseases, including MS and Parkinson’s. The next step is the use of VR systems, like Glass and Kinect, for personalized rehabilitation. 50 subjects, both healthy…