MIT CSAIL professor Regina Barzilay and Harvard/MGH professor Constance Lehman have developed a deep learning model that can predict breast cancer, from a mammogram, up to five years in the future. The model learned subtle breast tissue patterns that lead to malignant tumors from mammograms and known outcomes of 90,000 MGH patients.
The goal is to individualize screening and prevention programs.
Barzilay said that “rather than taking a one-size-fits-all approach, we can personalize screening around a woman’s risk of developing cancer. For example, a doctor might recommend that one group of women get a mammogram every other year, while another higher-risk group might get supplemental MRI screening.”
The algortithm accurately placed 31 percent of all cancer patients in its highest-risk category, compared to 18 percent for traditional models.
Lehman hopes to change screening strategies from age-based to risk based. “This is because before we did not have accurate risk assessment tools that worked for individual women.”
Current risk assement, based on age, family history of breast and ovarian cancer, hormonal and reproductive factors, and breast density, are weakly correlated with breast cancer. This makes many organizations believe that risk-based screening is not possible.
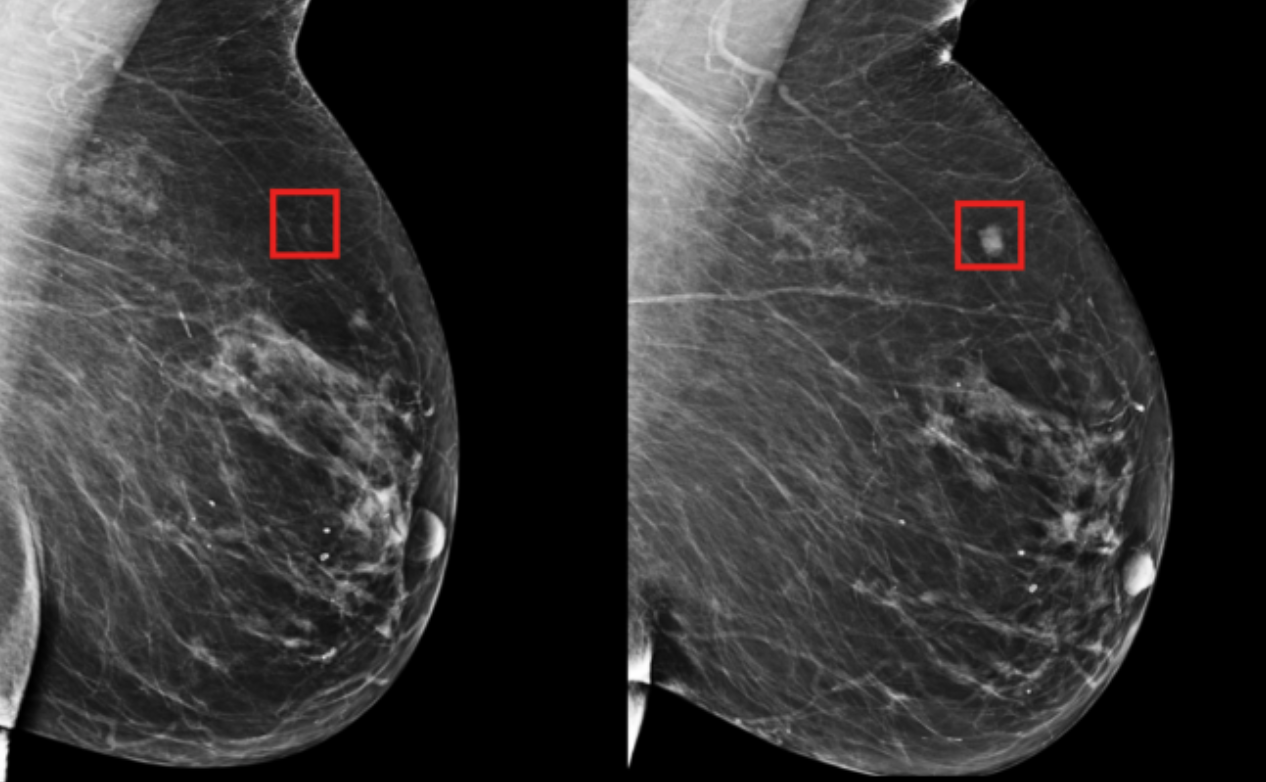
Rather than manually identifying the patterns in a mammogram that drive future cancer, the algorithm deduced patterns directly from the data, detecting abnormalities too subtle for the human eye to see.
Lehman said that “since the 1960s radiologists have noticed that women have unique and widely variable patterns of breast tissue visible on the mammogram. These patterns can represent the influence of genetics, hormones, pregnancy, lactation, diet, weight loss, and weight gain. We can now leverage this detailed information to be more precise in our risk assessment at the individual level.”
The MIT/MGH model is equally accurate for white and black women, as opposed to prior models. Black women have been shown to be 42 percent more likely to die from breast cancer due to a wide range of factors that may include differences in detection and access to health care.
Barzilay believes the system could, in the future, determine, based on mammograms, if patients are at a greater risk for cardiovascular disease or other cancers.
Professor Constance Lehman will discuss this technology at ApplySci’s 12th Wearable Tech + Digital Health + Neurotech Boston conference on November 14, 2019 at Harvard Medical School