Scientist-led conferences at Harvard, Stanford and MIT
-
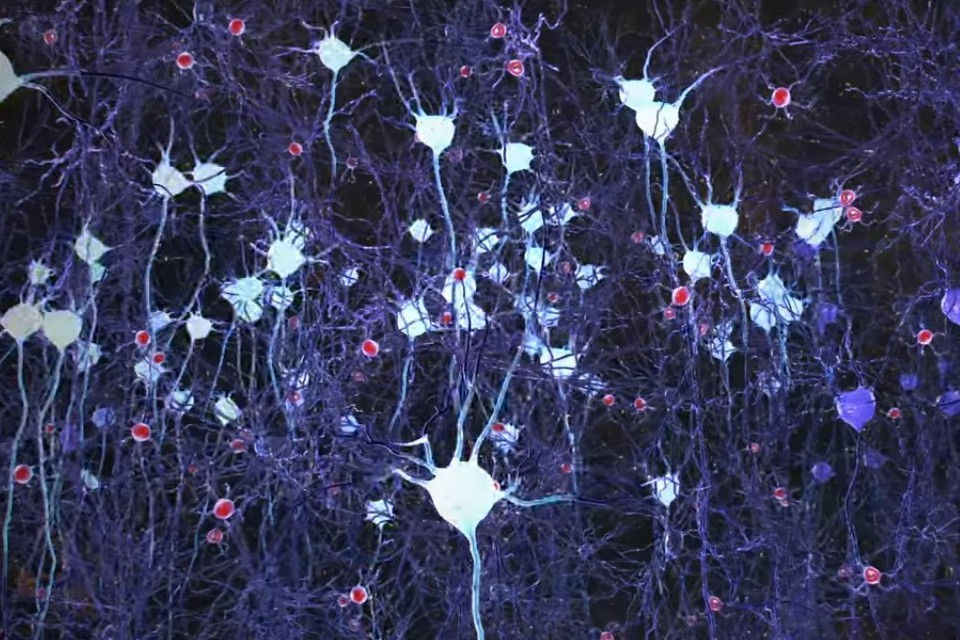
Non-invasive visual stimulation to treat Alzheimer’s disease
Cognito Therapeutics is developing a device-driven approach to Alzheimer’s treatment. Based on research by MIT’s Ed Boyden, globally recognized for his work in optogenetics, and Li-Hue Tsai, director of the Picower Institute for Learning and Memory, flickering-light stimulation has been used to restore gamma oscillation in the brains of the mice. This activated microglia cells to remove…
-

Sensors + robotics + AI for safer aging in place
IBM and rice University are developing MERA — a Waston enabled robot meant to help seniors age in place. The system comprises a Pepper robot interface, Watson, and Rice’s CameraVitals project, which calculates vital signs by recording video of a person’s face. Vitals are measured multiple times each day. Caregivers are informed if the the camera and/or accelerometer detect…
-
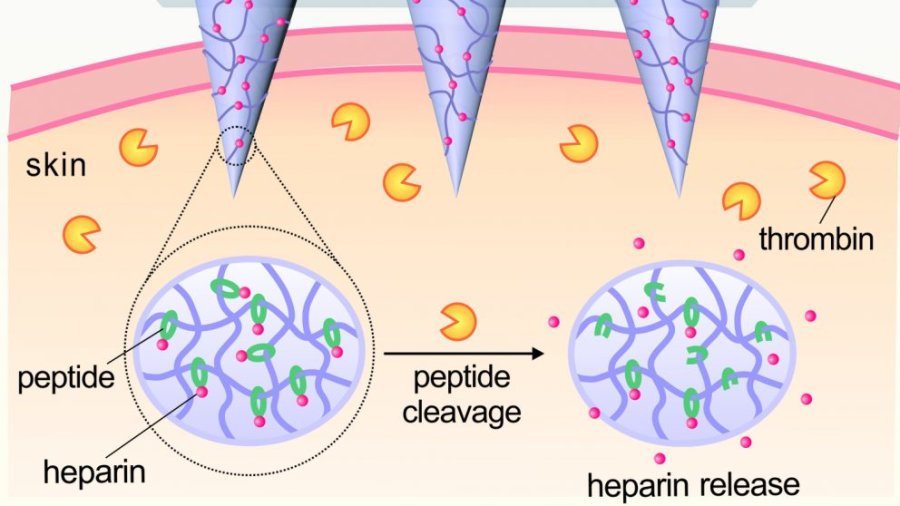
Self regulating patch optimizes blood thinner delivery
UNC and NC State researchers have developed a promising, self-regulating, Heparin releasing patch, meant to optimize levels of the blood thinner in one’s body. It has only been tested on animals, but was found to be more effective at preventing thrombosis than traditional drug delivery methods. Current protocol requires regular blood testing, to prevent hemorrhaging…
-
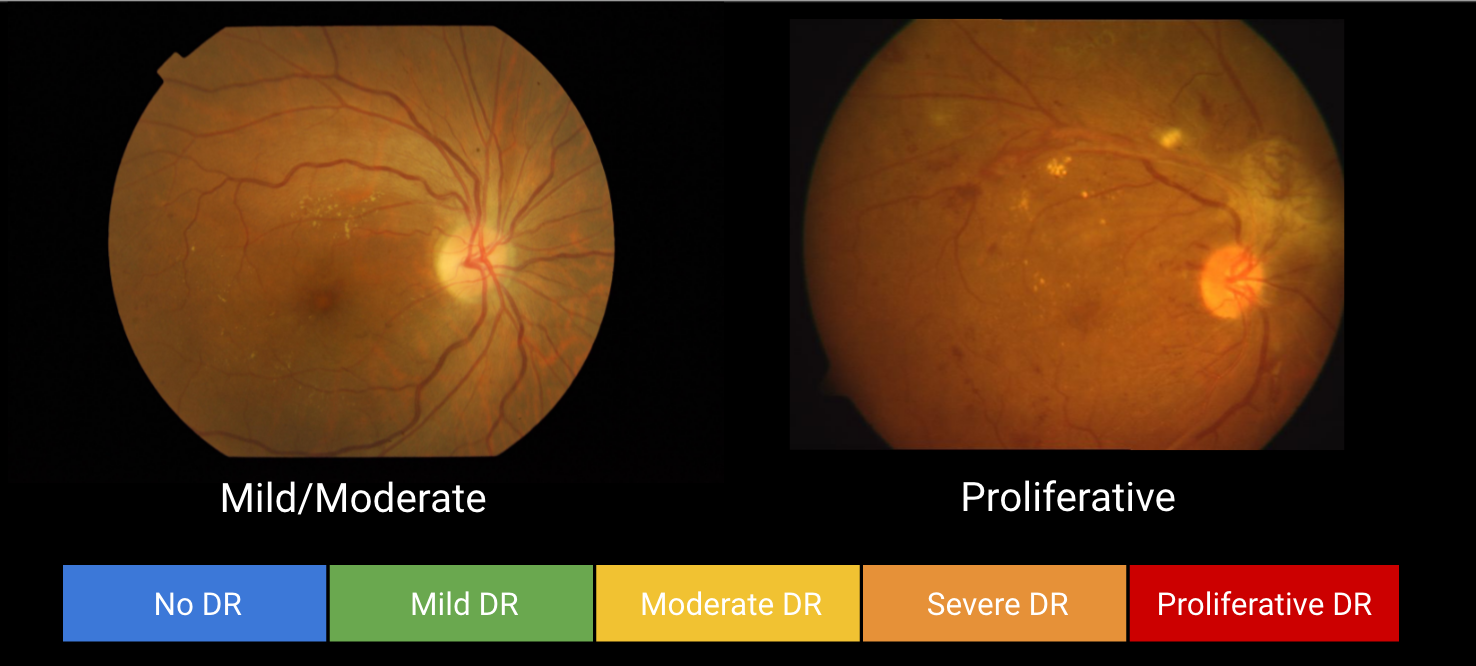
Diabetic retinopathy-detecting algorithm for remote diagnosis
Google has developed an algorithm which it claims is capable of detecting diabetic retinopathy in photographs. The goal is to improve the quality and availability of screening for, and early detection of, the common and debilitating condition. Typically, highly trained specialists are required to examine photos, to detect the lesions that indicate bleeding and fluid…
-
Cabin sensors, wearables, smart pills to monitor air passenger health
British Airlines has filed a patent application for a system that would monitor when a passenger is awake, asleep, hungry, nervous, hot, cold or uncomfortable. The “system and method for controlling the travel environment for a passenger” encompasses motion-sensing sleep monitors, wearables that track eye movement, heart rate, and temperature, and ingestible health-tracking pills. The…
-

Sensor sock detects diabetic inflammation, sends alerts
Siren Care‘s real-time temperature sensing smart sock is meant to detect foot inflammation in diabetics. The goal is early notification to prevent (difficult to heal) sores and other symptoms of the disease, which can lead to extreme complications. Data is stored in the fabric and in the cloud. An app sends alerts when a temperature event…
-
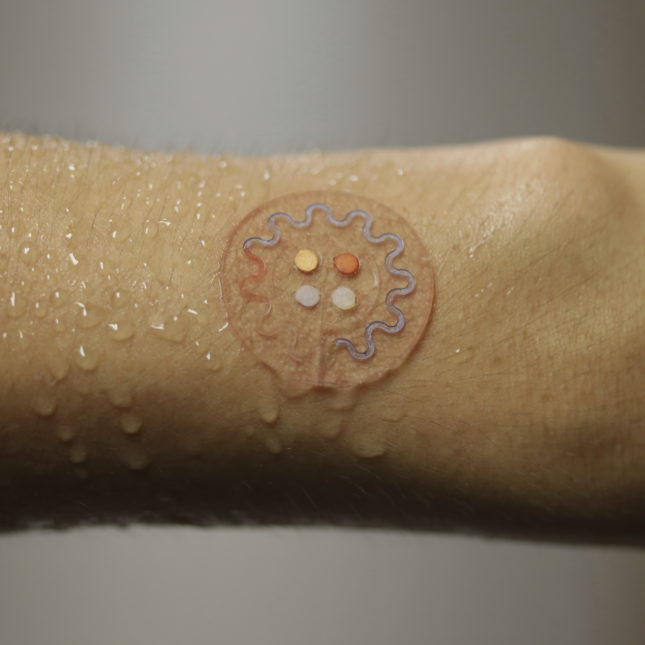
Wearable patch monitors lactate, glucose, and pH in sweat
Northwestern’s John Rogers has developed a wearable, sweat analyzing patch. The flexible microfluidic device uses colorimetric biochemical assays and integrates smartphone image capture analysis to monitor lactate, glucose, chloride ion concentrations, and pH. The wearable, with sports, military, and disease monitoring applications, can be adapted to test tears and saliva. Professor Rogers will be a…
-
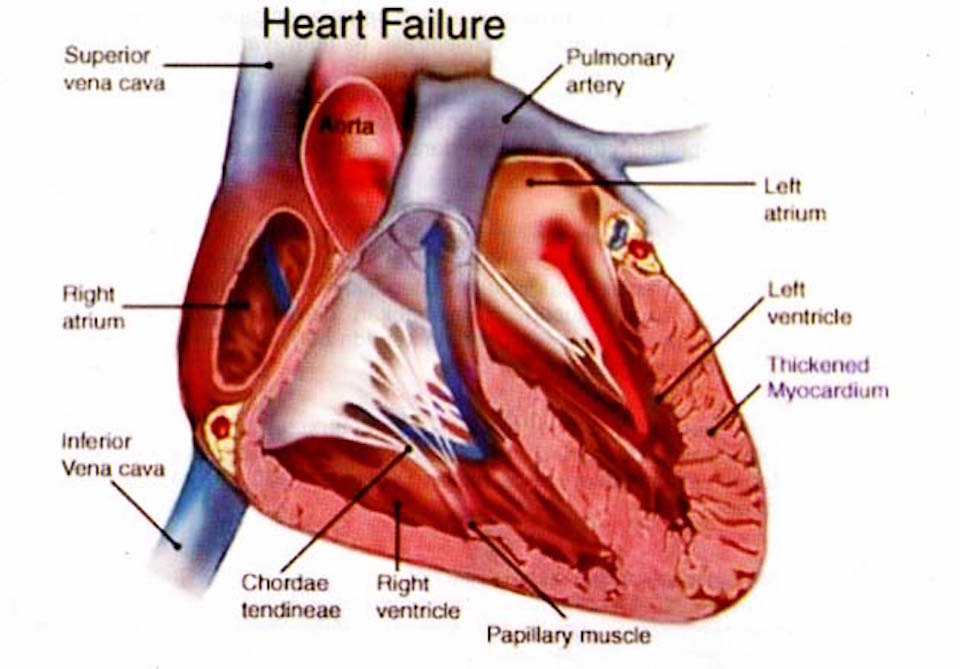
Implanted sensors predict heart failure events
Penn State’s John Boehmer used Boston Scientific’s HeartLogic sensors (retrofitted in already implanted devices) to track heart failure in a study of 900 patients. The goal was continuous monitoring and early event detection and prevention. Currently, heart failure is (not very successfully) managed by monitoring weight and reported symptoms. One in five patients are readmitted within 30…
-

Tiny sensor monitors the heart, recognizes speech, enables human-machine interfaces
Northwestern professor John Rogers has released a paper detailing his latest tiny, wearable, flexible, highly accurate health sensor, which monitors the heart, recognizes speech, and can enable human-machine interfaces. Professor Yonggang Huang is the corresponding author. The soft, continuous monitor adheres to any part of the body, detecting mechanical waves that propagate through tissues and fluids…
-
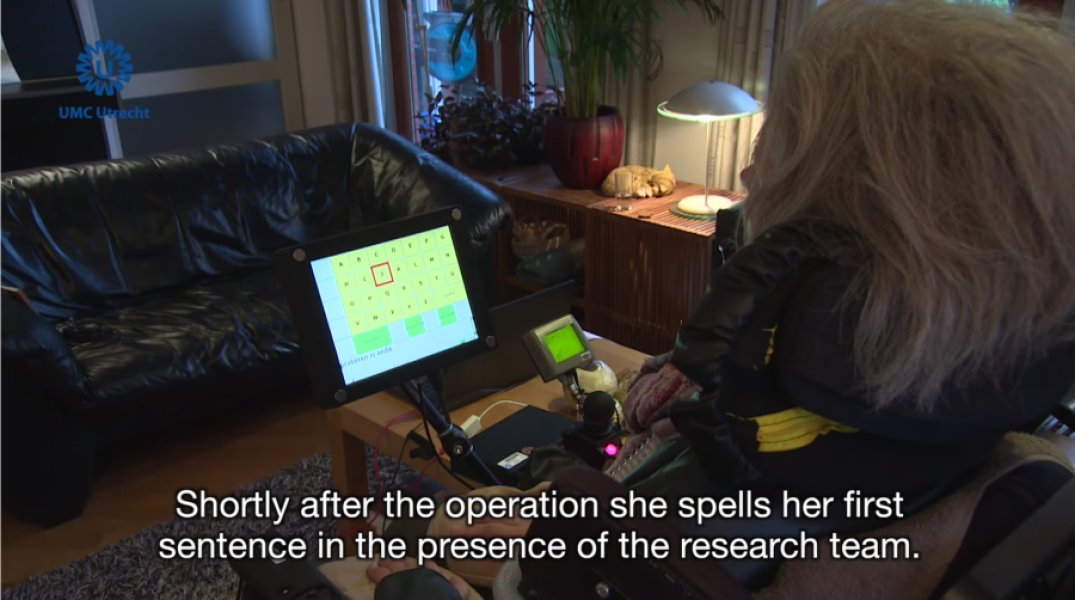
Implanted device enables slow, but more reliable, brain-driven typing
UMC Utrecht professor Nick Ramsey has developed an implantable brain computer interface that allowed a locked-in ALS patient to (very slowly) translate her thoughts into text. Until recently, the patient used eye tracking to spell words on a computer screen, as many ALS patients do. However, as 1/3 of patients lose the ability to control their eyes,…
-

Voice analysis as a diagnostic tool
Beyond Verbal recently used its emotion-detecting voice analysis app in an attempt to predict coronary artery disease in 150 study participants, 120 of whom had presented for angiography. The company claims to have identified 13 voice features associated with CAD – and one associated with a 19-fold increase in its likelihood. The researchers said that…
-

Science, not walls.
Reactionary politics must not deter our focus. On the future. On science. On technology. On healthcare. On progress. On our shared humanity. It is my honor to gather the brilliant, for interdisciplinary exchanges about improving health, treating disease, and assisting the disabled. About enhancing life. At our Digital Health + NeuroTech conferences at Stanford and MIT. Thank you…
Got any book recommendations?