Scientist-led conferences at Harvard, Stanford and MIT
-
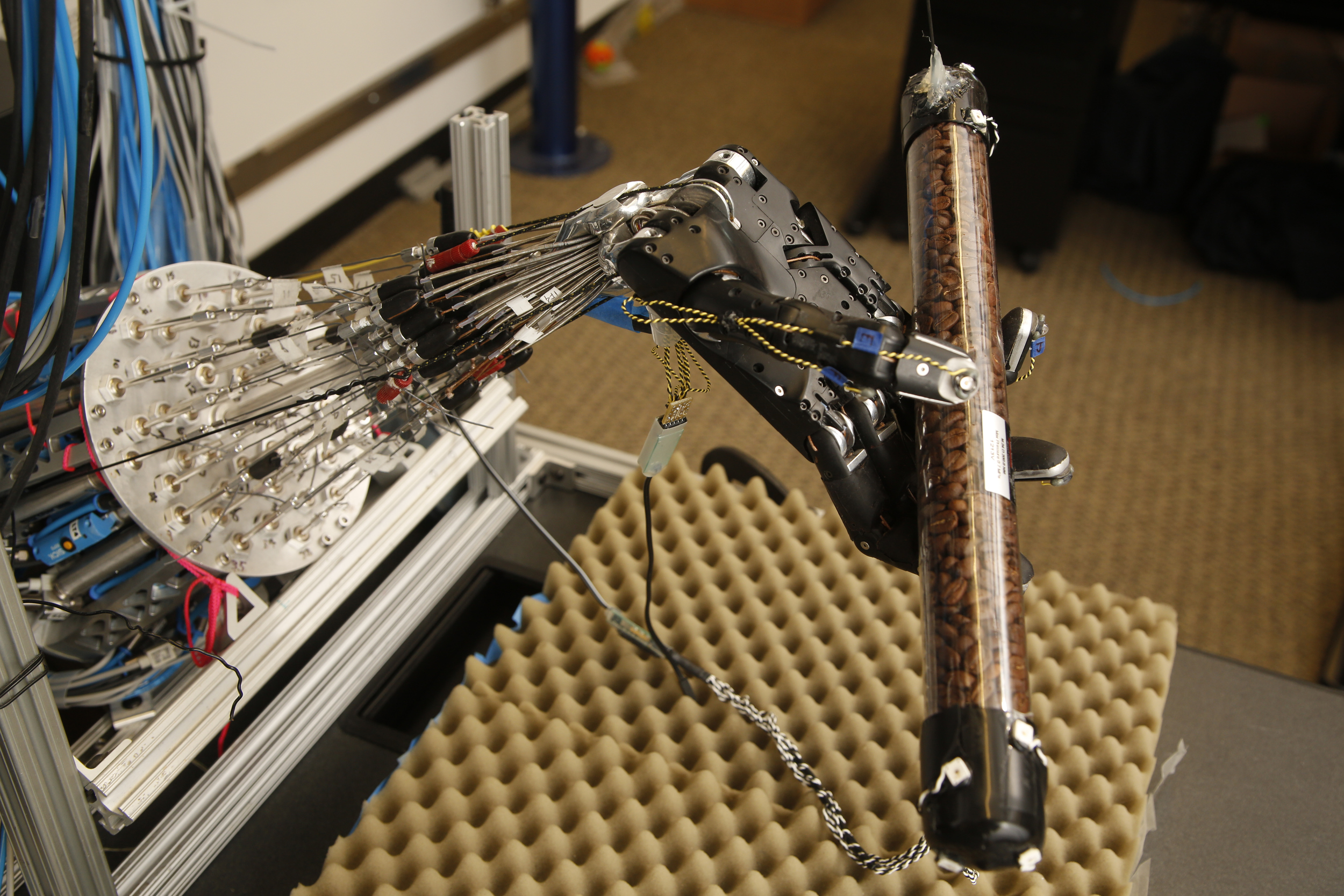
Machine learning model enables robotic hand to learn autonomously
Vikash Kumar and University of Washington colleagues have developed a simulation model that allows robotic hands to learn from their own experiences, while performing dexterous manipulation. Human direction is not required. A recent study incorporated the model while a robotic hand attempted several tasks, including rotating an elongated object. With each try, the hand became…
-
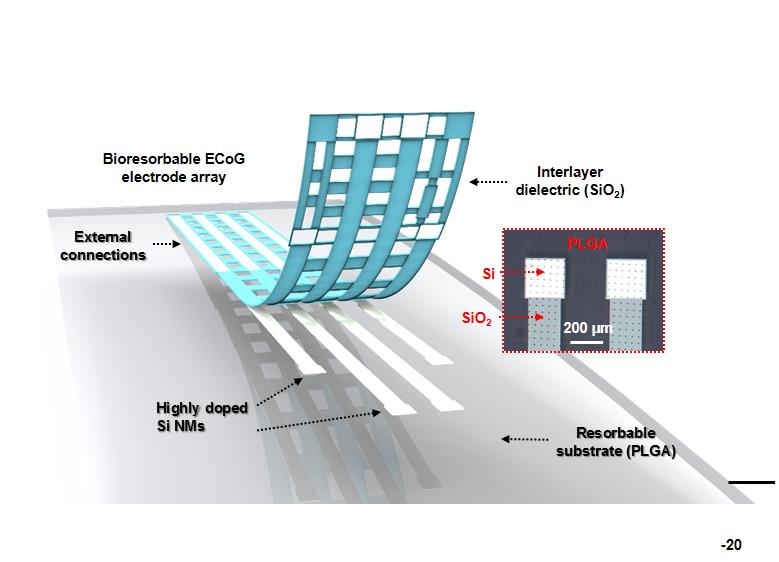
Self-dissolving brain monitoring electrodes
University of Pennsylvania researchers are developing implantable, brain monitoring electrodes that dissolve at a predetermined rate. The DARPA funded device could provide continuous data used to monitor or treat Parkinson’s disease, depression and chronic pain. As it is absorbed into the body, the risk associated with removal is eliminated. ApplySci recently described a related self…
-

Game navigation uncovers early dementia signs
Sea Hero Quest is a smartphone game that follows the journey of a sea explorer who has lost his memories. It is being used as a tool to uncover early dementia symptoms for research purposes. One of the first symptoms of dementia could be a loss of orientation. Gamer decisions and movements will help researchers…
-

“Cognitive Dress” colors reflect observer emotions
At the Met Gala, New York’s most sought-after invitation, Karolina Kurkova wore a Marchesa dress that was powered by IBM Watson to react to social media sentiment in real-time. The “Cognitive Dress” was covered in LED embedded fabric flowers that lit in colors to reflect joy, passion, excitement, encouragement and curiosity, as expressed on twitter.…
-

Lung function analyzed via phone, from anywhere
Mayank Goel and University of Washington colleagues have developed SpiroCall, a system that measures lung function by analyzing a caller’s voice via smartphone, landline or payphone microphone. An algorithm uses the phone microphone as an uncalibrated pressure sensor. Captured audio is converted into an estimate of the flow-rate of air exiting from a patient’s mouth.…
-
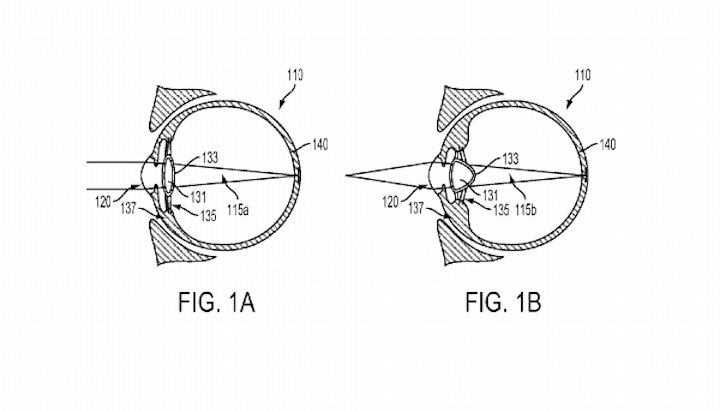
Vision enhancing, injectable smart lens
Google has filed a patent for a vision enhancing, injectable smart lens. The “intraocular device” is meant to replace one’s natural lens, and focus light onto the eye’s retina. It is injected into the eye in a solution that congeals and attaches to the lens capsule. It will contain its own storage, and tiny radio components that…
-

Non-invasive electric field treatment for glioblastoma
Optune by Novocure uses targeted electric fields to disrupt cancer cell division and cause cancer cell death. 500 hospitals globally can prescribe the FDA approved treatment to glioblastoma patients. “Tumor Treating Fields” are low intensity, alternating electric fields within the intermediate frequency range. TTFields disrupt cell division through physical interactions with key molecules during mitosis.…
-
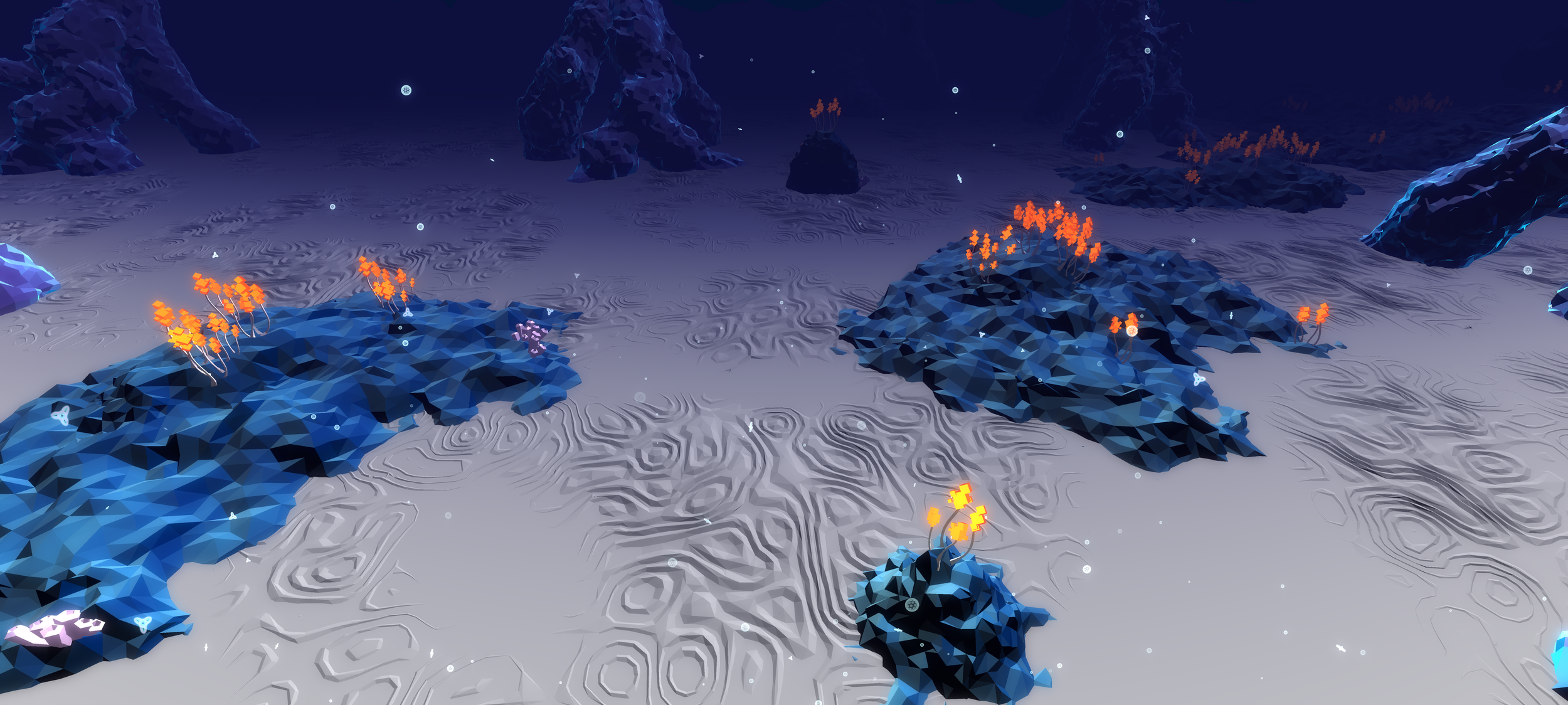
Anxiety reducing VR game
Deep VR teaches breathing techniques meant to reduce the anxiety of users during a game. Its developers believe that the skills learned can also help manage stress during daily life. It is the basis of a Radboud University study, in the lab of Isabela Granic, that aims to alleviate anxiety in children. 100 children have…
-
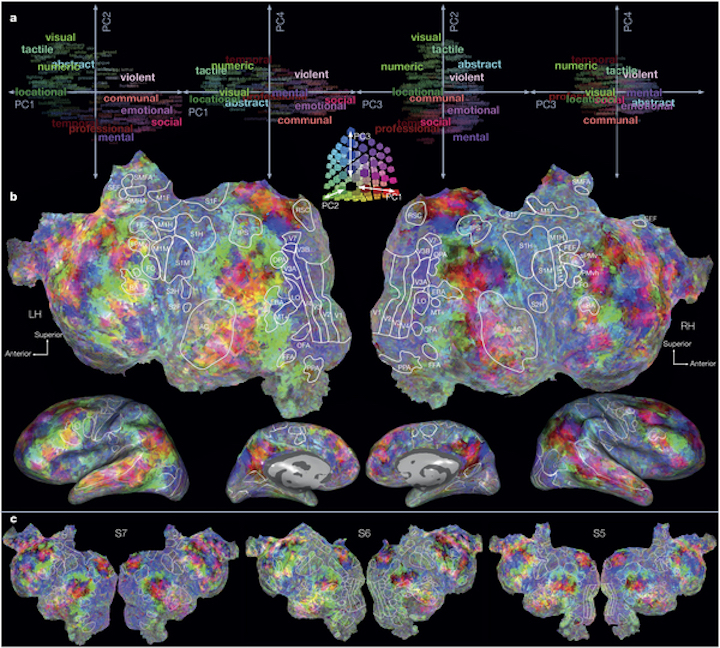
Semantic brain atlas created with fMRI
Jack Gallant and Berkeley colleagues have used fMRI to understand how language-related information is represented and processed in the human brain. Brain blood flow changes were measured once every second, as subjects listened to natural narrative stories. Mathematical models and big data analysis were used to create detailed maps, showing how different aspects of language…
-

Sports camera collects, overlays health data
As part of its new developer program, GoPro has partnered with Polar to overlay health data on videos. Similar to video games, sports videos will be able to display heart rate, speed, distance, and altitude. This has been presented as a fun feature, but could also provide physicians with a better understanding of one’s health in various…
-
Heart monitoring patch tracks patients post-discharge
BeVITAL by Vital Connect, in partnership with BePatient, is a clinical grade, continuous, heart monitoring wearable, and data sharing system, for the early detection of abnormalities post-discharge. The thin, disposable patch adheres to the chest, and tracks heart activity, breathing, temperature, movement, posture, and falls. It can be used for 4 days, and transmits data to a…
-

“Mixed Reality” headset could support surgery, rehab, learning
Magic Leap has unveiled its “mixed reality” headset, where virtual objects are integrated into the real world. In addition to obvious gaming and entertainment applications, the system could be used in healthcare (including in surgery, surgery preparation, and orthopedic rehabilitation) and education. The company remains vague in its description of its technology, but head and…
Got any book recommendations?