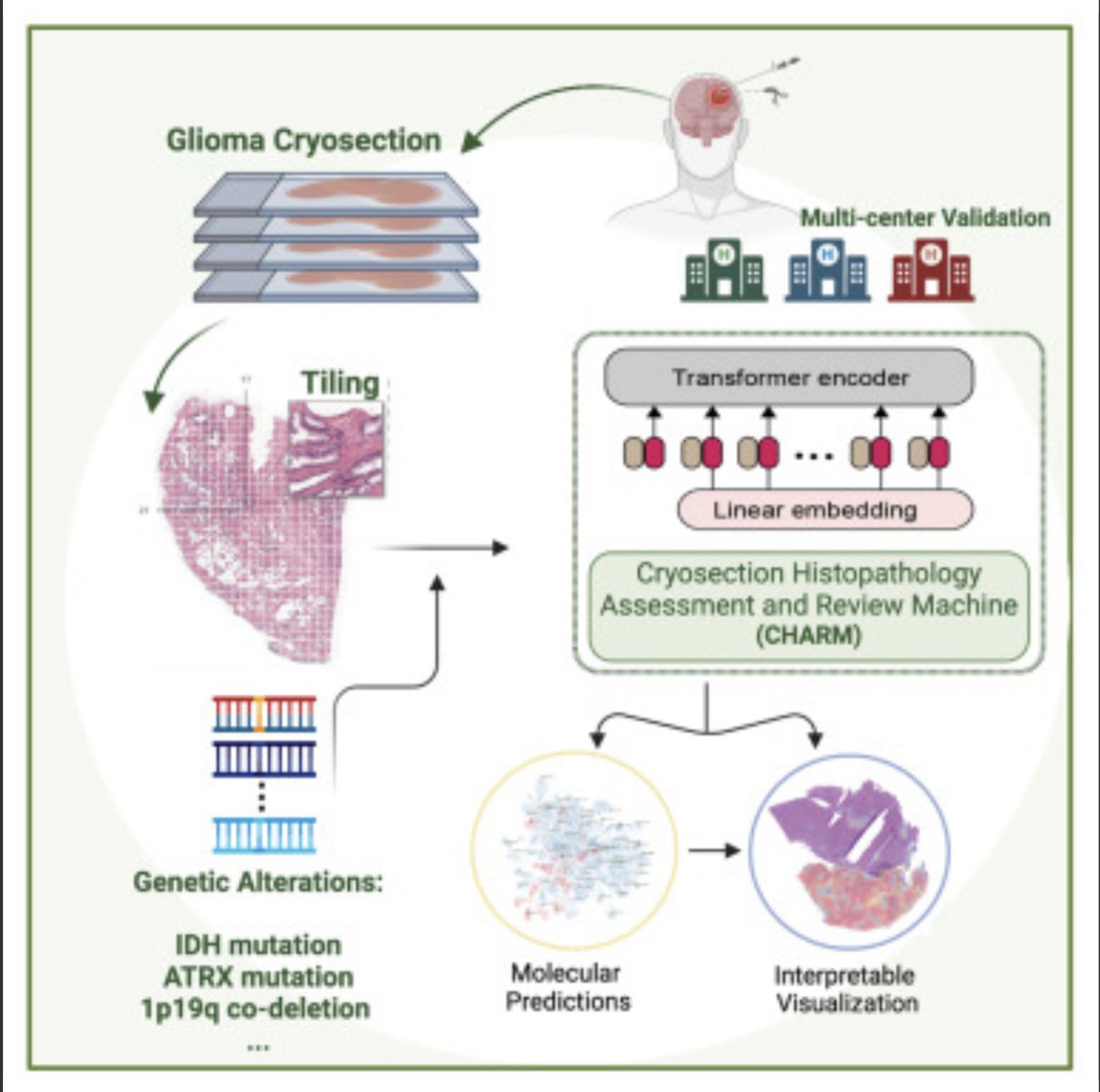
Kun-Hsing Yu and HMS colleagues used AI to rapidly determine a brain tumor’s molecular identity during surgery, propeling the development of precision oncology. The tool is CHARM (Cryosection Histopathology Assessment and Review Machine.) Currently, genetic sequencing takes days to weeks.
Accurate molecular diagnosis during surgery can help a neurosurgeon decide how much brain tissue to remove. Removing too much when the tumor is less aggressive can affect a patient’s neurologic and cognitive function. Removing too little when the tumor is highly aggressive may leave behind malignant tissue that can grow and spread quickly.
The technology will also allow the surgeon to determine if the patient can benefit from immediate treatment with drug-coated wafers placed directly into the brain at the time of the operation.
The standard intraoperative diagnostic approach used now involves taking brain tissue, freezing it, and examining it under a microscope. A major drawback is that freezing the tissue tends to alter the appearance of cells under a microscope and can interfere with the accuracy of clinical evaluation. Furthermore, the human eye, even when using potent microscopes, cannot reliably detect subtle genomic variations on a slide.
The new AI approach overcomes these challenges and could be particularly valuable in areas with limited access to technology to perform rapid cancer genetic sequencing.
Knowledge of a tumor’s molecular type provides insight about its aggressiveness, behavior, and likely response to various treatments, which can inform post-operative decisions.
The new tool enables during-surgery diagnoses aligned with the WHO classification system for diagnosing and grading the severity of gliomas, which calls for such diagnoses to be made based on a tumor’s genomic profile.
CHARM was developed using 2,334 brain tumor samples from 1,524 people with glioma from three different patient populations. When tested on a never-before-seen set of brain samples, the tool distinguished tumors with specific molecular mutations at 93 percent accuracy and successfully classified three major types of gliomas with distinct molecular features that carry different prognoses and respond differently to treatments.
It successfully captured visual characteristics of the tissue surrounding the malignant cells. It was capable of spotting telltale areas with greater cellular density and more cell death within samples, both of which signal more aggressive glioma types.
CHARM was also able to pinpoint clinically important molecular alterations in a subset of low-grade gliomas, a subtype of glioma that is less aggressive and therefore less likely to invade surrounding tissue. Each of these changes also signals different propensity for growth, spread, and treatment response.
It further connected the appearance of the cells — the shape of their nuclei, the presence of edema around the cells — with the molecular profile of the tumor. This means that the algorithm can pinpoint how a cell’s appearance relates to the molecular type of a tumor.
Accorging to Yu, this ability to assess the broader context around the image renders the model more accurate and closer to how a human pathologist would visually assess a tumor sample.
The researchers said that while the model was trained and tested on glioma samples, it could be successfully retrained to identify other brain cancer subtypes.
Scientists have already designed AI models to profile other types of cancer — colon, lung, breast — but gliomas have remained particularly challenging due to their molecular complexity and huge variation in tumor cells’ shape and appearance.
The CHARM tool would have to be retrained periodically to reflect new disease classifications as they emerge from new knowledge. “Just like human clinicians who must engage in ongoing education and training, AI tools must keep up with the latest knowledge to remain at peak performance,” according to Yu.
Join ApplySci at MIT on September 18, 2023 for the 14th AI + Deep Tech Health + Neurotech conference.